[2]
Badalahu, Qin B, Luo J, Zeng Y, Fu S, Zhang L. Classification of the subtalar articular surface and its matching situation: an anatomical study on Chinese subtalar joint. Surgical and radiologic anatomy : SRA. 2020 Oct:42(10):1133-1139. doi: 10.1007/s00276-020-02444-4. Epub 2020 Feb 28
[PubMed PMID: 32112282]
Level 2 (mid-level) evidence
[4]
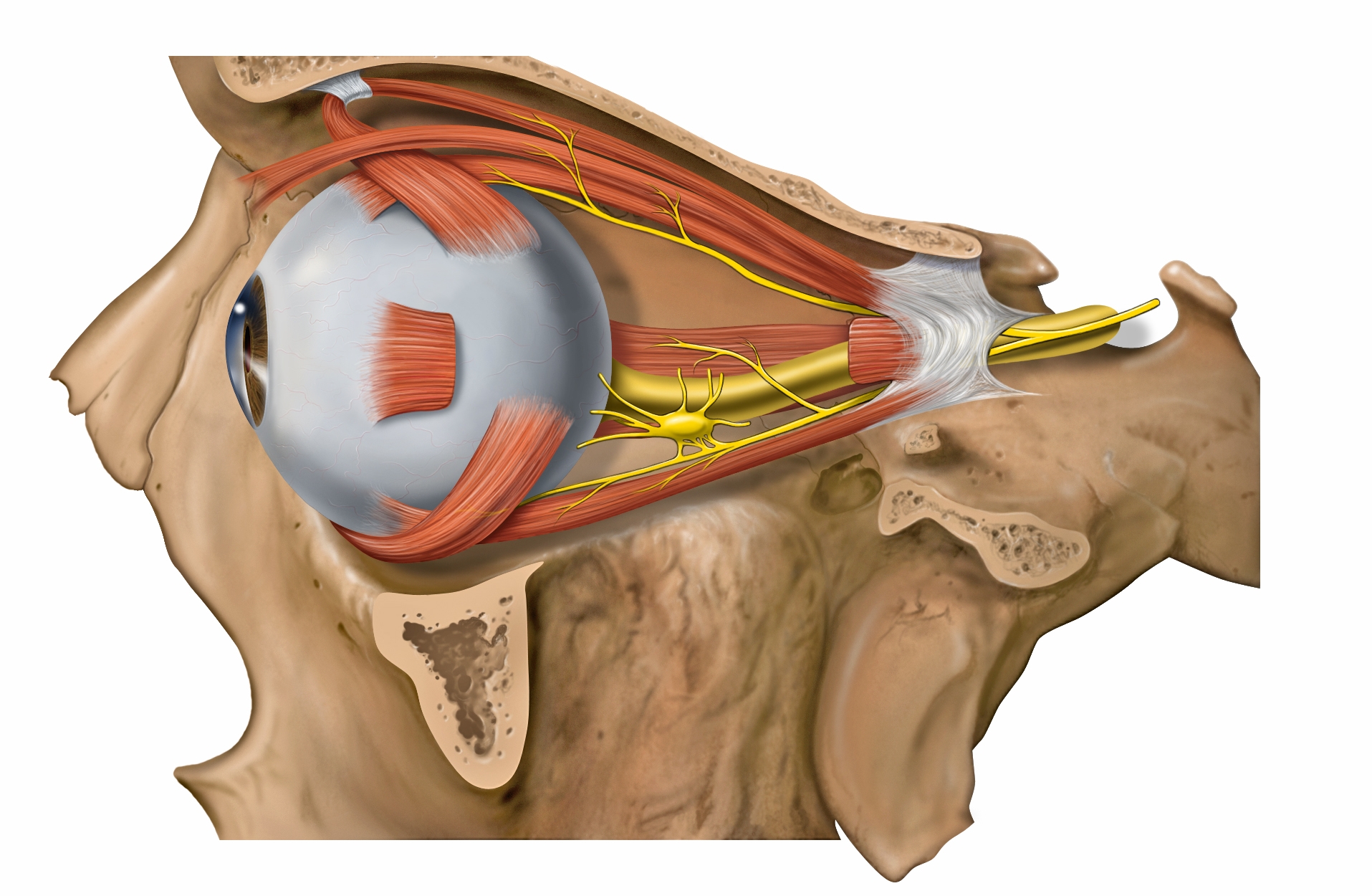
Abdelhady A, Patel BC, Aslam S, Al Aboud DM. Anatomy, Head and Neck: Eye Superior Oblique Muscle. StatPearls. 2023 Jan:():
[PubMed PMID: 30725837]
[6]
Chung IH, Han J, Iwata J, Chai Y. Msx1 and Dlx5 function synergistically to regulate frontal bone development. Genesis (New York, N.Y. : 2000). 2010 Nov:48(11):645-55. doi: 10.1002/dvg.20671. Epub 2010 Nov 2
[PubMed PMID: 20824629]
[7]
Tyler MS. Development of the frontal bone and cranial meninges in the embryonic chick: an experimental study of tissue interactions. The Anatomical record. 1983 May:206(1):61-70
[PubMed PMID: 6881551]
[8]
Katori Y, Rodríguez-Vázquez JF, Kawase T, Murakami G, Cho BH, Abe S. Early fetal development of hard tissue pulleys for the human superior oblique and tensor veli palatini muscles. Annals of anatomy = Anatomischer Anzeiger : official organ of the Anatomische Gesellschaft. 2011 Mar:193(2):127-33. doi: 10.1016/j.aanat.2011.01.004. Epub 2011 Jan 26
[PubMed PMID: 21334866]
[9]
Rodríguez-Vázquez JF, Honkura Y, Katori Y, Murakami G, Abe H. Fetal development of the pulley for muscle insertion tendons: A review and new findings related to the tensor tympani tendon. Annals of anatomy = Anatomischer Anzeiger : official organ of the Anatomische Gesellschaft. 2017 Jan:209():1-10. doi: 10.1016/j.aanat.2016.09.001. Epub 2016 Sep 29
[PubMed PMID: 27693602]
[10]
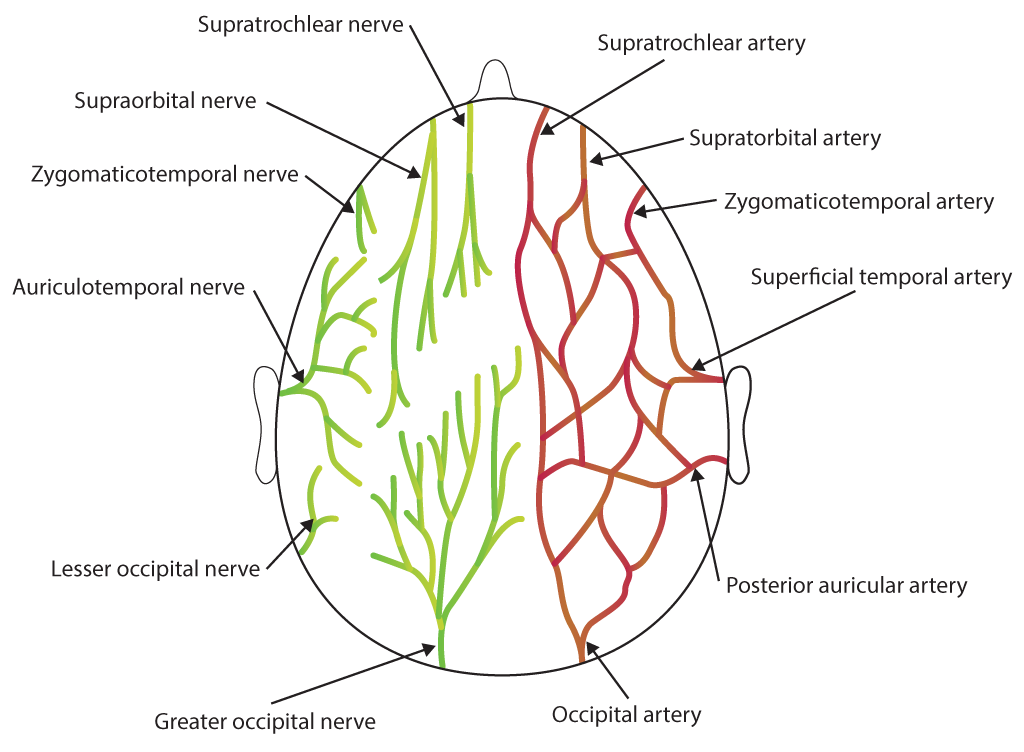
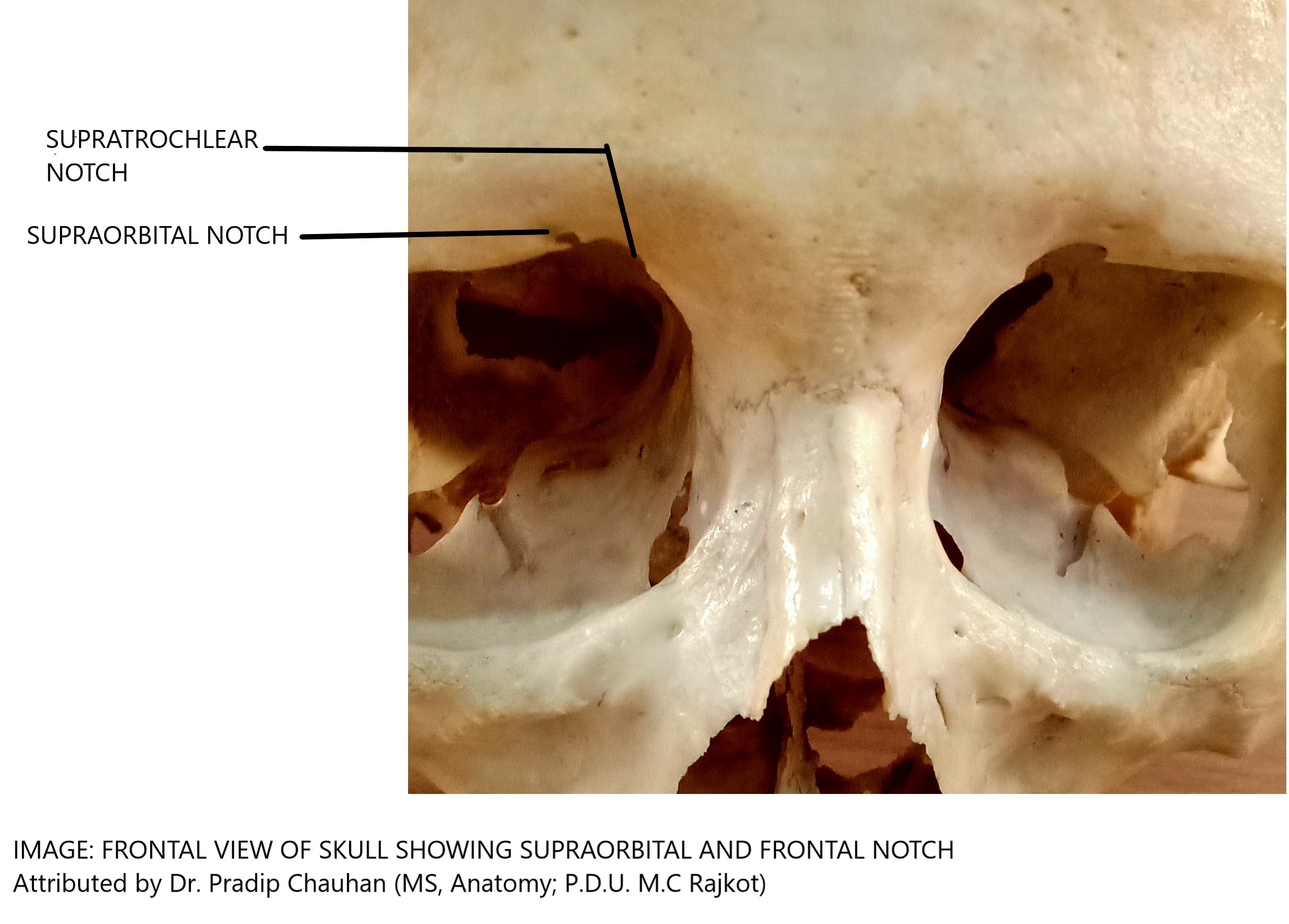
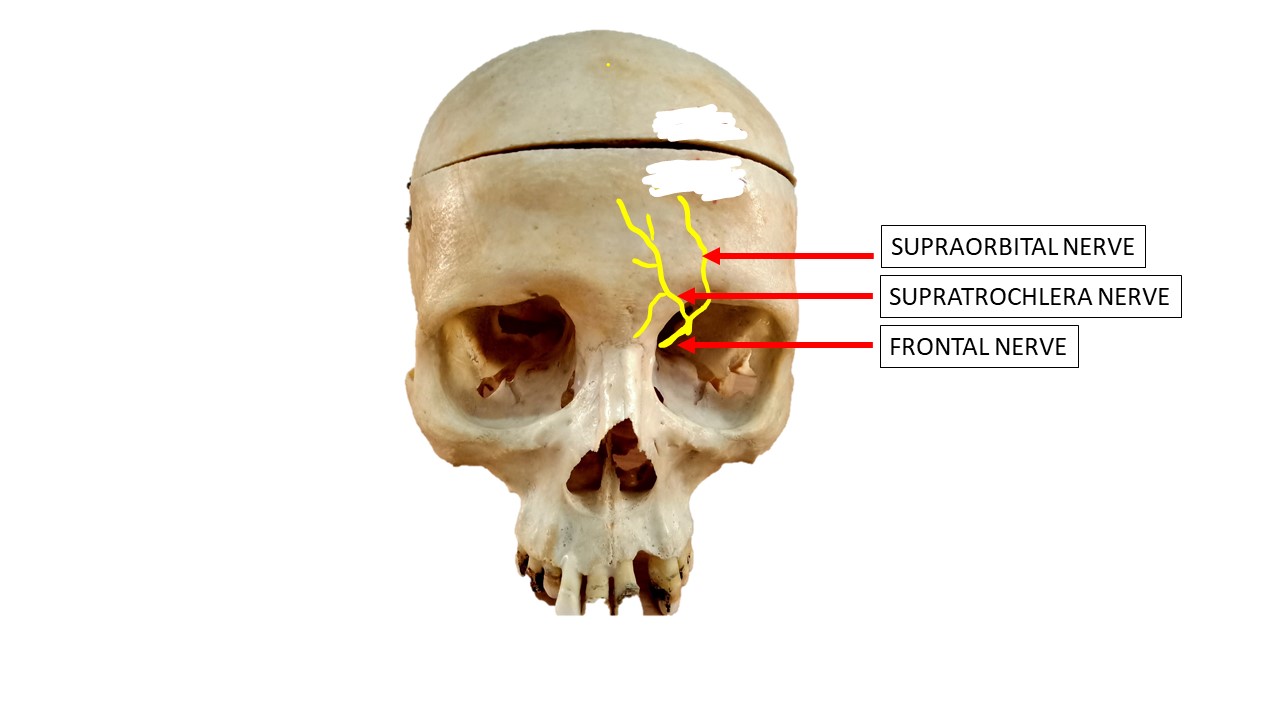
Haładaj R, Polguj M, Topol M. Anatomical Variations of the Supraorbital and Supratrochlear Nerves: Their Intraorbital Course and Relation to the Supraorbital Margin. Medical science monitor : international medical journal of experimental and clinical research. 2019 Jul 13:25():5201-5210. doi: 10.12659/MSM.915447. Epub 2019 Jul 13
[PubMed PMID: 31301129]
[11]
Freter S, Fleenor SJ, Freter R, Liu KJ, Begbie J. Cranial neural crest cells form corridors prefiguring sensory neuroblast migration. Development (Cambridge, England). 2013 Sep:140(17):3595-600. doi: 10.1242/dev.091033. Epub
[PubMed PMID: 23942515]
[12]
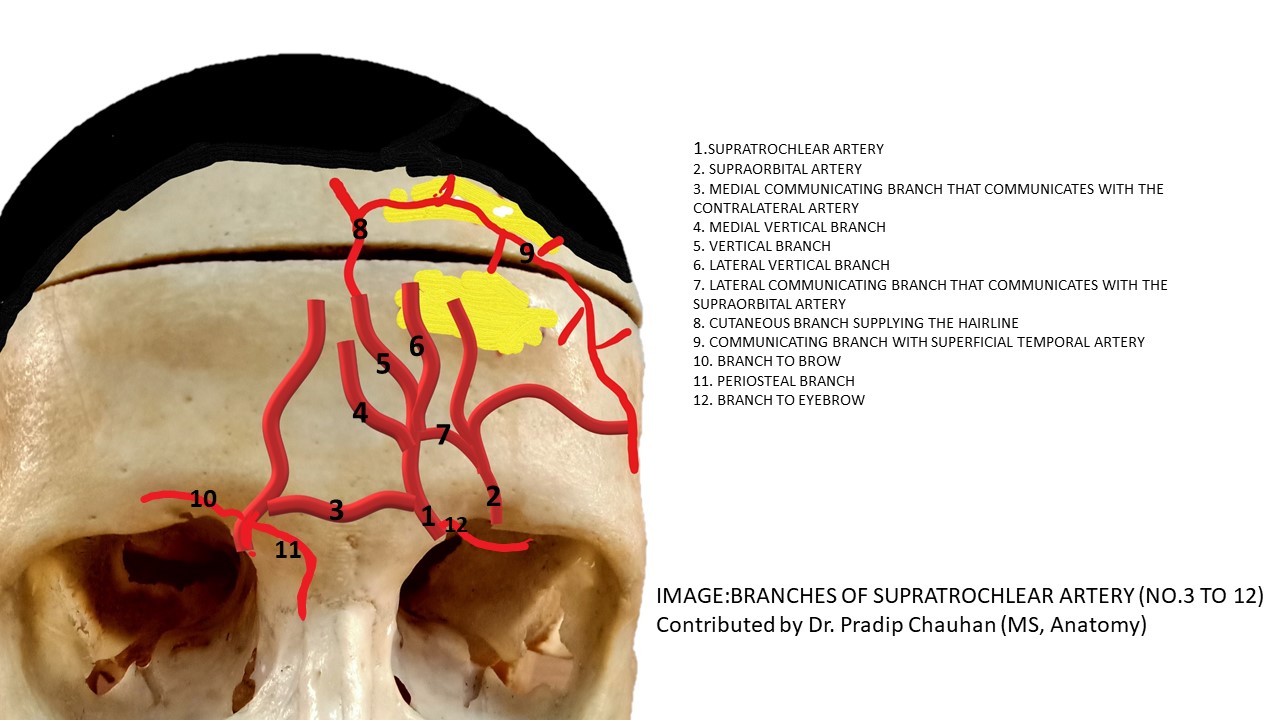
Agorgianitis L, Panagouli E, Tsakotos G, Tsoucalas G, Filippou D. The Supratrochlear Artery Revisited: An Anatomic Review in Favor of Modern Cosmetic Applications in the Area. Cureus. 2020 Feb 29:12(2):e7141. doi: 10.7759/cureus.7141. Epub 2020 Feb 29
[PubMed PMID: 32257686]
[13]
Shumrick KA, Smith TL. The anatomic basis for the design of forehead flaps in nasal reconstruction. Archives of otolaryngology--head & neck surgery. 1992 Apr:118(4):373-9
[PubMed PMID: 1554465]
[15]
Kleintjes WG. Forehead anatomy: arterial variations and venous link of the midline forehead flap. Journal of plastic, reconstructive & aesthetic surgery : JPRAS. 2007:60(6):593-606
[PubMed PMID: 17485046]
[16]
Cai XY, Li ZM, Xu YB, Cheng G, Luo P. [The anatomic features of supratrochlear artery]. Zhonghua zheng xing wai ke za zhi = Zhonghua zhengxing waike zazhi = Chinese journal of plastic surgery. 2009 Nov:25(6):456-9
[PubMed PMID: 20209940]
[17]
Brodland DG. Paramedian forehead flap reconstruction for nasal defects. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.]. 2005 Aug:31(8 Pt 2):1046-52
[PubMed PMID: 16042928]
[19]
Cai X, Li Z. [Applied anatomy study of supratrochlear vein in reconstruction of nasal defect]. Zhongguo xiu fu chong jian wai ke za zhi = Zhongguo xiufu chongjian waike zazhi = Chinese journal of reparative and reconstructive surgery. 2009 Feb:23(2):219-21
[PubMed PMID: 19275108]
[20]
Janis JE, Hatef DA, Hagan R, Schaub T, Liu JH, Thakar H, Bolden KM, Heller JB, Kurkjian TJ. Anatomy of the supratrochlear nerve: implications for the surgical treatment of migraine headaches. Plastic and reconstructive surgery. 2013 Apr:131(4):743-750. doi: 10.1097/PRS.0b013e3182818b0c. Epub
[PubMed PMID: 23249981]
[21]
Gras-Cabrerizo JR, Martel-Martin M, Garcia-Lorenzo J, Rodríguez-Álvarez F, Montserrat-Gili JR, Mirapeix-Lucas R, Massegur-Solench H. Surgical Anatomy of the Medial Wall of the Orbit in 14 Human Cadavers. Journal of neurological surgery. Part B, Skull base. 2016 Dec:77(6):439-444
[PubMed PMID: 27857868]
[22]
Ortiz R, Gfrerer L, Hansdorfer MA, Nealon KP, Lans J, Austen WG Jr. Migraine Surgery at the Frontal Trigger Site: An Analysis of Intraoperative Anatomy. Plastic and reconstructive surgery. 2020 Feb:145(2):523-530. doi: 10.1097/PRS.0000000000006475. Epub
[PubMed PMID: 31985652]
[23]
Kikuta S, Yalcin B, Iwanaga J, Watanabe K, Kusukawa J, Tubbs RS. The supraorbital and supratrochlear nerves for ipsilateral corneal neurotization: anatomical study. Anatomy & cell biology. 2020 Mar:53(1):2-7. doi: 10.5115/acb.19.147. Epub 2019 Mar 31
[PubMed PMID: 32274242]
[24]
Olinevich VB, Ziangirova GG. [Embryogenesis and structural-and-functional specificity of corneal nerves in health and pathology]. Vestnik oftalmologii. 2004 Jul-Aug:120(4):47-50
[PubMed PMID: 15384854]
[25]
Eghrari AO, Riazuddin SA, Gottsch JD. Overview of the Cornea: Structure, Function, and Development. Progress in molecular biology and translational science. 2015:134():7-23. doi: 10.1016/bs.pmbts.2015.04.001. Epub 2015 Jun 4
[PubMed PMID: 26310146]
Level 3 (low-level) evidence
[26]
Konschake M, Burger F, Zwierzina M. Peripheral Nerve Anatomy Revisited: Modern Requirements for Neuroimaging and Microsurgery. Anatomical record (Hoboken, N.J. : 2007). 2019 Aug:302(8):1325-1332. doi: 10.1002/ar.24125. Epub 2019 Apr 16
[PubMed PMID: 30951264]
[27]
Bradford BD, Lee JW. Reconstruction of the Forehead and Scalp. Facial plastic surgery clinics of North America. 2019 Feb:27(1):85-94. doi: 10.1016/j.fsc.2018.08.009. Epub
[PubMed PMID: 30420075]
[28]
Shin A, Yoo L, Chaudhuri Z, Demer JL. Independent passive mechanical behavior of bovine extraocular muscle compartments. Investigative ophthalmology & visual science. 2012 Dec 19:53(13):8414-23. doi: 10.1167/iovs.12-10318. Epub 2012 Dec 19
[PubMed PMID: 23188730]
[29]
Pauzenberger R, Pikula R, Berchtold V, Mühlbacher J, Rieger UM. Anatomy of the supratrochlear nerve: implications for the surgical treatment of migraine headaches. Plastic and reconstructive surgery. 2014 May:133(5):723e-724e. doi: 10.1097/PRS.0000000000000137. Epub
[PubMed PMID: 24776587]
[30]
Turhan-Haktanir N, Ayçiçek A, Haktanir A, Demir Y. Variations of supraorbital foramina in living subjects evaluated with multidetector computed tomography. Head & neck. 2008 Sep:30(9):1211-5. doi: 10.1002/hed.20866. Epub
[PubMed PMID: 18642294]
[31]
Domeshek LF, Hunter DA, Santosa K, Couch SM, Ali A, Borschel GH, Zuker RM, Snyder-Warwick AK. Anatomic characteristics of supraorbital and supratrochlear nerves relevant to their use in corneal neurotization. Eye (London, England). 2019 Mar:33(3):398-403. doi: 10.1038/s41433-018-0222-0. Epub 2018 Sep 27
[PubMed PMID: 30262895]
[32]
Konofaos P, Soto-Miranda MA, Ver Halen J, Fleming JC. Supratrochlear and supraorbital nerves: an anatomical study and applications in the head and neck area. Ophthalmic plastic and reconstructive surgery. 2013 Sep-Oct:29(5):403-8. doi: 10.1097/IOP.0b013e318295fa09. Epub
[PubMed PMID: 23928468]
[33]
Erdogmus S, Govsa F. Anatomy of the supraorbital region and the evaluation of it for the reconstruction of facial defects. The Journal of craniofacial surgery. 2007 Jan:18(1):104-12
[PubMed PMID: 17251847]
[34]
Sertel S, Pasche P. Pericranial Flap for Inner Lining in Nasal Reconstruction. Annals of plastic surgery. 2016 Oct:77(4):425-32. doi: 10.1097/SAP.0000000000000624. Epub
[PubMed PMID: 26418782]
[35]
Park SS. Reconstruction of nasal defects larger than 1.5 centimeters in diameter. The Laryngoscope. 2000 Aug:110(8):1241-50
[PubMed PMID: 10942120]
[36]
Sadashivam S. Isolated Orbital Roof Fracture: Can It Be Catastrophic? Asian journal of neurosurgery. 2018 Jul-Sep:13(3):935-937. doi: 10.4103/ajns.AJNS_101_18. Epub
[PubMed PMID: 30283587]
[37]
Liu H, Hu S, Qin W. Traumatic prolapse of the globe into the anterior cranial fossa: a case report. BMC ophthalmology. 2020 Apr 3:20(1):128. doi: 10.1186/s12886-020-01403-2. Epub 2020 Apr 3
[PubMed PMID: 32245433]
Level 2 (mid-level) evidence
[38]
Lopez J, Pineault K, Pradeep T, Khavanin N, Kachniarz B, Faateh M, Grant MP, Redett RJ, Manson PN, Dorafshar AH. Pediatric Frontal Bone and Sinus Fractures: Cause, Characteristics, and a Treatment Algorithm. Plastic and reconstructive surgery. 2020 Apr:145(4):1012-1023. doi: 10.1097/PRS.0000000000006645. Epub
[PubMed PMID: 32221225]
[39]
Lofrese G, Mongardi L, De Bonis P, Scerrati A, Nicassio N, Cultrera F. Spontaneous Repositioning of Isolated Blow-In Orbital Roof Fracture: Could Wait and See Be a Strategy in Asymptomatic Cases? The Journal of craniofacial surgery. 2020 May/Jun:31(3):e263-e266. doi: 10.1097/SCS.0000000000006231. Epub
[PubMed PMID: 32049903]
Level 3 (low-level) evidence
[40]
Gómez Roselló E, Quiles Granado AM, Artajona Garcia M, Juanpere Martí S, Laguillo Sala G, Beltrán Mármol B, Pedraza Gutiérrez S. Facial fractures: classification and highlights for a useful report. Insights into imaging. 2020 Mar 19:11(1):49. doi: 10.1186/s13244-020-00847-w. Epub 2020 Mar 19
[PubMed PMID: 32193796]
[41]
Salam GA. Regional anesthesia for office procedures: part I. Head and neck surgeries. American family physician. 2004 Feb 1:69(3):585-90
[PubMed PMID: 14971840]
[42]
Herlich A. Focused local anesthesia and analgesia for head and neck surgery. International anesthesiology clinics. 2012 Winter:50(1):13-25. doi: 10.1097/AIA.0b013e318218f6ee. Epub
[PubMed PMID: 22227420]
[43]
Novitch M, Hyatali FS, Jeha G, Motejunas M, Bonneval L, Pankaj T, Cornett EM, Jones MR, Kaye RJ, Urman RD, Kaye AD. Regional techniques for head and neck surgical procedures. Best practice & research. Clinical anaesthesiology. 2019 Dec:33(4):377-386. doi: 10.1016/j.bpa.2019.06.004. Epub 2019 Jul 2
[PubMed PMID: 31791557]
[44]
Lee HJ, Choi KS, Won SY, Apinuntrum P, Hu KS, Kim ST, Tansatit T, Kim HJ. Topographic Relationship between the Supratrochlear Nerve and Corrugator Supercilii Muscle--Can This Anatomical Knowledge Improve the Response to Botulinum Toxin Injections in Chronic Migraine? Toxins. 2015 Jul 17:7(7):2629-38. doi: 10.3390/toxins7072629. Epub 2015 Jul 17
[PubMed PMID: 26193317]
[45]
Filipović B, de Ru JA, van de Langenberg R, Borggreven PA, Lacković Z, Lohuis PJFM. Decompression endoscopic surgery for frontal secondary headache attributed to supraorbital and supratrochlear nerve entrapment: a comprehensive review. European archives of oto-rhino-laryngology : official journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS) : affiliated with the German Society for Oto-Rhino-Laryngology - Head and Neck Surgery. 2017 May:274(5):2093-2106. doi: 10.1007/s00405-017-4450-x. Epub 2017 Jan 25
[PubMed PMID: 28124109]
[46]
Gfrerer L, Guyuron B. Surgical treatment of migraine headaches. Acta neurologica Belgica. 2017 Mar:117(1):27-32. doi: 10.1007/s13760-016-0731-1. Epub 2016 Dec 24
[PubMed PMID: 28013487]
[47]
Khan TT, Colon-Acevedo B, Mettu P, DeLorenzi C, Woodward JA. An Anatomical Analysis of the Supratrochlear Artery: Considerations in Facial Filler Injections and Preventing Vision Loss. Aesthetic surgery journal. 2017 Feb:37(2):203-208. doi: 10.1093/asj/sjw132. Epub 2016 Aug 16
[PubMed PMID: 27530765]
[48]
Cho KH, Dalla Pozza E, Toth G, Bassiri Gharb B, Zins JE. Pathophysiology Study of Filler-Induced Blindness. Aesthetic surgery journal. 2019 Jan 1:39(1):96-106. doi: 10.1093/asj/sjy141. Epub
[PubMed PMID: 29873688]
[49]
Li X, Du L, Lu JJ. A Novel Hypothesis of Visual Loss Secondary to Cosmetic Facial Filler Injection. Annals of plastic surgery. 2015 Sep:75(3):258-60. doi: 10.1097/SAP.0000000000000572. Epub
[PubMed PMID: 26207560]
[50]
Allali J, Bernard A, Assaraf E, Bourges JL, Renard G. [Multiple embolizations of the branches of the ophthalmic artery: an unknown serious complication of facial surgeries]. Journal francais d'ophtalmologie. 2006 Jan:29(1):51-7
[PubMed PMID: 16465125]
[51]
Wu S, Pan L, Wu H, Shi H, Zhao Y, Ji Y, Zeng H. Anatomic Study of Ophthalmic Artery Embolism Following Cosmetic Injection. The Journal of craniofacial surgery. 2017 Sep:28(6):1578-1581. doi: 10.1097/SCS.0000000000003674. Epub
[PubMed PMID: 28749836]