Introduction
Radiation safety is a concern for patients, physicians, and staff in many departments, including radiology, interventional cardiology, and surgery. Radiation emitted during fluoroscopic procedures is responsible for the greatest radiation dose for medical staff. Radiation from diagnostic imaging modalities, such as computed tomography, mammography, and nuclear imaging, are minor contributors to the cumulative dose exposures of healthcare personnel. However, any radiation exposure poses a potential risk to both patients and healthcare workers alike.[1]
Radiation protection aims to reduce unnecessary radiation exposure with a goal to minimize the harmful effects of ionizing radiation.[2] In the medical field, ionizing radiation has become an inescapable tool used for the diagnosis and treatment of a variety of medical conditions. As its use has evolved, so have the cumulative doses of lifetime radiation that both patients and medical providers receive. Most radiation exposure in medical settings arises from fluoroscopic imaging, which uses x-rays to obtain dynamic and cinematic functional imaging. Formal radiation protection training helps reduce radiation exposure to medical staff and patients.[3] However, enforcing radiation safety guidelines can be an arduous process, and many interventionalists do not receive formal training in either residency or fellowship on radiation dose reduction. In particular, clinicians or medical staff that use fluoroscopic imaging outside of dedicated radiology or interventional departments have low adherence to radiation safety guidelines. Fluoroscopy is used in many specialties, including orthopedics, urology, interventional radiology, interventional cardiology, vascular surgery, and gastroenterology. As radiation exposure becomes more prevalent, a thorough understanding of radiation exposure risks and dose reduction techniques will be of utmost importance.
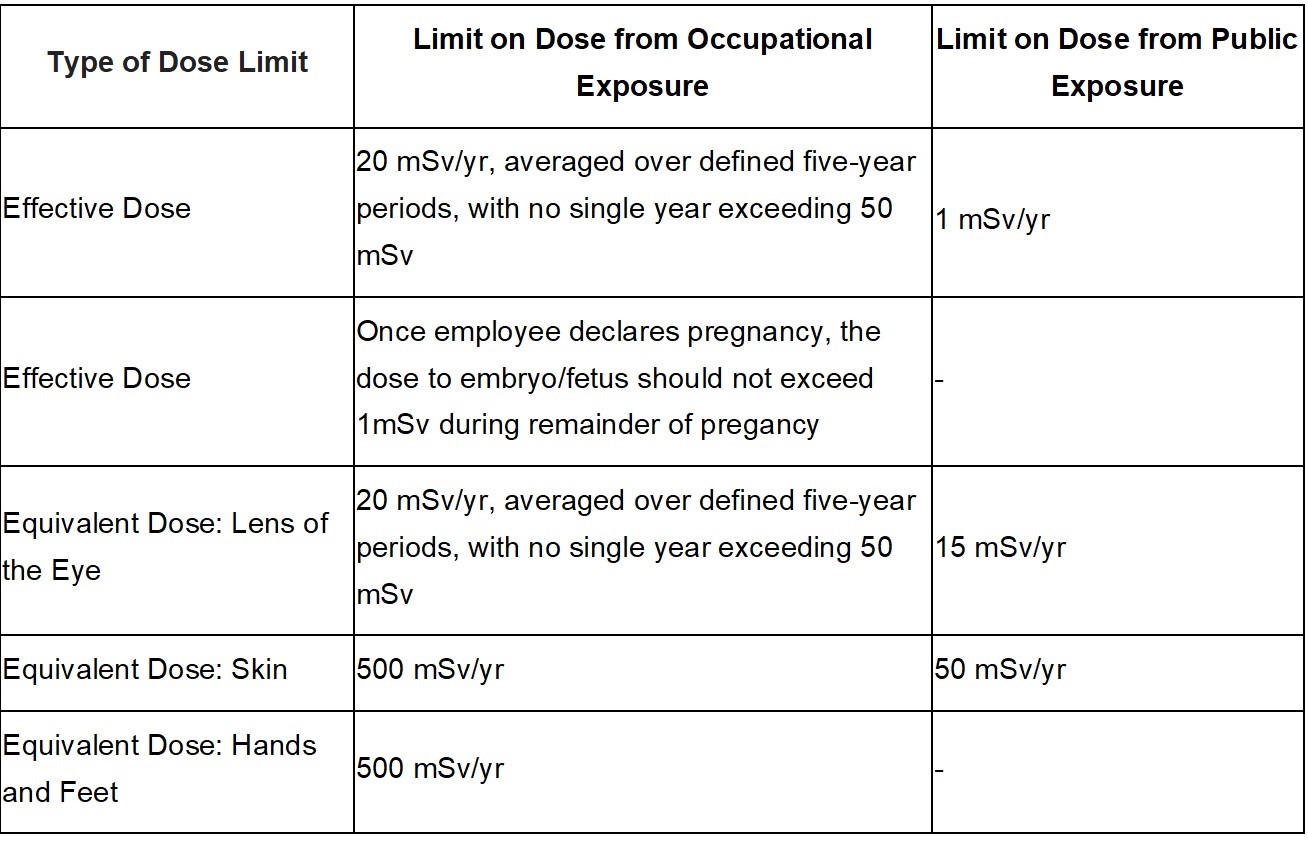
There are three basic principles of radiation protection: justification, optimization, and dose limitation. Justification involves an appreciation for the benefits and risks of using radiation for procedures or treatments. Physicians, surgeons, and radiologic personnel all play a key role in educating patients on the potential adverse effects of radiation exposure. The benefits of exposure should be well known and accepted by the medical community. Often, procedures that expose patients to relatively higher doses of radiation—for example, interventional vascular procedures—are medically necessary, and thus the benefits outweigh the risks. The As Low as Reasonably Achievable (ALARA) principle, defined by the code of federal regulations, was created to ensure that all measures to reduce radiation exposure have been taken while acknowledging that radiation is an integral part of diagnosing and treating patients. Any amount of radiation exposure will increase the risk of stochastic effects, namely the chances of developing malignancy following radiation exposure. These effects are thought to occur as a linear model in which there is no specific threshold to predict whether or not malignancy will develop reliably. For these reasons, the radiologic community teaches protection practices under the ALARA principle.