[1]
Liu G, Wang H, Le J, Lan L, Xu Y, Yang Y, Chen J, Han F. Early-stage predictors for treatment responses in patients with active lupus nephritis. Lupus. 2019 Mar:28(3):283-289. doi: 10.1177/0961203319826703. Epub 2019 Jan 25
[PubMed PMID: 30682900]
[2]
Slight-Webb S, Guthridge JM, Chakravarty EF, Chen H, Lu R, Macwana S, Bean K, Maecker HT, Utz PJ, James JA. Mycophenolate mofetil reduces STAT3 phosphorylation in systemic lupus erythematosus patients. JCI insight. 2019 Jan 24:4(2):. doi: 10.1172/jci.insight.124575. Epub 2019 Jan 24
[PubMed PMID: 30674728]
[3]
Wang ZR, Ren LM, Li R, Guan X, Han QM, Liu ML, Shao M, Zhang X, Chen S, Li ZG. [Analysis of 20-year survival rate and prognostic indicators of systemic lupus erythematosus]. Zhonghua yi xue za zhi. 2019 Jan 15:99(3):178-182. doi: 10.3760/cma.j.issn.0376-2491.2019.03.005. Epub
[PubMed PMID: 30669759]
[4]
Wilson HR, Medjeral-Thomas NR, Gilmore AC, Trivedi P, Seyb K, Farzaneh-Far R, Gunnarsson I, Zickert A, Cairns TD, Lightstone L, Cook HT, Pickering MC. Glomerular membrane attack complex is not a reliable marker of ongoing C5 activation in lupus nephritis. Kidney international. 2019 Mar:95(3):655-665. doi: 10.1016/j.kint.2018.09.027. Epub 2019 Jan 14
[PubMed PMID: 30655025]
[5]
Tamirou F, Houssiau FA. Management of Lupus Nephritis. Journal of clinical medicine. 2021 Feb 9:10(4):. doi: 10.3390/jcm10040670. Epub 2021 Feb 9
[PubMed PMID: 33572385]
[6]
Houssiau FA, Ginzler EM. Current treatment of lupus nephritis. Lupus. 2008 May:17(5):426-30. doi: 10.1177/0961203308090029. Epub
[PubMed PMID: 18490421]
[7]
Parikh SV, Almaani S, Brodsky S, Rovin BH. Update on Lupus Nephritis: Core Curriculum 2020. American journal of kidney diseases : the official journal of the National Kidney Foundation. 2020 Aug:76(2):265-281. doi: 10.1053/j.ajkd.2019.10.017. Epub 2020 Mar 24
[PubMed PMID: 32220510]
[8]
Iwamoto T, Niewold TB. Genetics of human lupus nephritis. Clinical immunology (Orlando, Fla.). 2017 Dec:185():32-39. doi: 10.1016/j.clim.2016.09.012. Epub 2016 Sep 28
[PubMed PMID: 27693588]
[9]
Su X, Yu H, Lei Q, Chen X, Tong Y, Zhang Z, Yang W, Guo Y, Lin L. Systemic lupus erythematosus: pathogenesis and targeted therapy. Molecular biomedicine. 2024 Oct 30:5(1):54. doi: 10.1186/s43556-024-00217-8. Epub 2024 Oct 30
[PubMed PMID: 39472388]
[10]
Munroe ME, James JA. Genetics of Lupus Nephritis: Clinical Implications. Seminars in nephrology. 2015 Sep:35(5):396-409. doi: 10.1016/j.semnephrol.2015.08.002. Epub
[PubMed PMID: 26573543]
[11]
Pan Q, Guo F, Huang Y, Li A, Chen S, Chen J, Liu HF, Pan Q. Gut Microbiota Dysbiosis in Systemic Lupus Erythematosus: Novel Insights into Mechanisms and Promising Therapeutic Strategies. Frontiers in immunology. 2021:12():799788. doi: 10.3389/fimmu.2021.799788. Epub 2021 Dec 3
[PubMed PMID: 34925385]
[12]
Skopelja-Gardner S, Tai J, Sun X, Tanaka L, Kuchenbecker JA, Snyder JM, Kubes P, Mustelin T, Elkon KB. Acute skin exposure to ultraviolet light triggers neutrophil-mediated kidney inflammation. Proceedings of the National Academy of Sciences of the United States of America. 2021 Jan 19:118(3):. doi: 10.1073/pnas.2019097118. Epub
[PubMed PMID: 33397815]
[13]
Bai H, Jiang L, Li T, Liu C, Zuo X, Liu Y, Hu S, Sun L, Zhang M, Lin J, Xiao W, Wang Q, Zhao D, Wu H, Kong X, Gao W, Hou W, Seong M, Zhang Y, Chen F, Chen S, Wu X, Bao C, Wang L, Xu H. Acute effects of air pollution on lupus nephritis in patients with systemic lupus erythematosus: A multicenter panel study in China. Environmental research. 2021 Apr:195():110875. doi: 10.1016/j.envres.2021.110875. Epub 2021 Feb 13
[PubMed PMID: 33592226]
[14]
López P, Sánchez B, Margolles A, Suárez A. Intestinal dysbiosis in systemic lupus erythematosus: cause or consequence? Current opinion in rheumatology. 2016 Sep:28(5):515-22. doi: 10.1097/BOR.0000000000000309. Epub
[PubMed PMID: 27466725]
Level 3 (low-level) evidence
[15]
Monticolo M, Mucha K, Foroncewicz B. Lupus Nephritis and Dysbiosis. Biomedicines. 2023 Apr 13:11(4):. doi: 10.3390/biomedicines11041165. Epub 2023 Apr 13
[PubMed PMID: 37189783]
[16]
Azzouz D, Omarbekova A, Heguy A, Schwudke D, Gisch N, Rovin BH, Caricchio R, Buyon JP, Alekseyenko AV, Silverman GJ. Lupus nephritis is linked to disease-activity associated expansions and immunity to a gut commensal. Annals of the rheumatic diseases. 2019 Jul:78(7):947-956. doi: 10.1136/annrheumdis-2018-214856. Epub 2019 Feb 19
[PubMed PMID: 30782585]
[17]
Quaglia M, Merlotti G, De Andrea M, Borgogna C, Cantaluppi V. Viral Infections and Systemic Lupus Erythematosus: New Players in an Old Story. Viruses. 2021 Feb 11:13(2):. doi: 10.3390/v13020277. Epub 2021 Feb 11
[PubMed PMID: 33670195]
[18]
Roveta A, Parodi EL, Brezzi B, Tunesi F, Zanetti V, Merlotti G, Francese A, Maconi AG, Quaglia M. Lupus Nephritis from Pathogenesis to New Therapies: An Update. International journal of molecular sciences. 2024 Aug 18:25(16):. doi: 10.3390/ijms25168981. Epub 2024 Aug 18
[PubMed PMID: 39201667]
[19]
Yung S, Chan TM. Anti-DNA antibodies in the pathogenesis of lupus nephritis--the emerging mechanisms. Autoimmunity reviews. 2008 Feb:7(4):317-21. doi: 10.1016/j.autrev.2007.12.001. Epub 2007 Dec 26
[PubMed PMID: 18295737]
[20]
Strizzi CT, Ambrogio M, Zanoni F, Bonerba B, Bracaccia ME, Grandaliano G, Pesce F. Epitope Spreading in Immune-Mediated Glomerulonephritis: The Expanding Target. International journal of molecular sciences. 2024 Oct 16:25(20):. doi: 10.3390/ijms252011096. Epub 2024 Oct 16
[PubMed PMID: 39456878]
[21]
Bruschi M, Angeletti A, Prunotto M, Meroni PL, Ghiggeri GM, Zeus consortium, Moroni G, Sinico RA, Franceschini F, Fredi M, Vaglio A, Cavalli A, Scapozza L, Patel JJ, Tan JC, Lo KC, Cavagna L, Petretto A, Pratesi F, Migliorini P, Locatelli F, Pazzola G, Pesce G, Giannese D, Manfredi A, Ramirez GA, Esposito P, Murdaca G, Negrini S, Bui F, Trezzi B, Emmi G, Cavazzana I, Binda V, Fenaroli P, Pisan I, Montecucco C, Santoro D, Scolari F, Mescia F, Volpi S, Mosca M, Tincani A, Ravelli A, Murtas C, Candiano G, Caridi G, La Porta E, Verrina E. A critical view on autoantibodies in lupus nephritis: Concrete knowledge based on evidence. Autoimmunity reviews. 2024 May:23(5):103535. doi: 10.1016/j.autrev.2024.103535. Epub 2024 Mar 27
[PubMed PMID: 38552995]
[22]
Zervopoulou E, Grigoriou M, Doumas SA, Yiannakou D, Pavlidis P, Gasparoni G, Walter J, Filia A, Gakiopoulou H, Banos A, Mitroulis I, Boumpas DT. Enhanced medullary and extramedullary granulopoiesis sustain the inflammatory response in lupus nephritis. Lupus science & medicine. 2024 Mar 11:11(1):. doi: 10.1136/lupus-2023-001110. Epub 2024 Mar 11
[PubMed PMID: 38471723]
[23]
Hong S, Healy H, Kassianos AJ. The Emerging Role of Renal Tubular Epithelial Cells in the Immunological Pathophysiology of Lupus Nephritis. Frontiers in immunology. 2020:11():578952. doi: 10.3389/fimmu.2020.578952. Epub 2020 Sep 23
[PubMed PMID: 33072122]
[24]
Luo M, Lıu J, Yuan Y, Chen Y, Yuan G. The role of vitamin D-synthesizing enzyme CYP27B1 in systemic lupus erythematosus. Turkish journal of medical sciences. 2022 Aug:52(4):984-989
[PubMed PMID: 36326421]
[25]
Kaneko M, Jackson SW. Recent advances in immunotherapies for lupus nephritis. Pediatric nephrology (Berlin, Germany). 2023 Apr:38(4):1001-1012. doi: 10.1007/s00467-022-05670-7. Epub 2022 Jul 1
[PubMed PMID: 35778517]
Level 3 (low-level) evidence
[26]
Brunner HI, Gladman DD, Ibañez D, Urowitz MD, Silverman ED. Difference in disease features between childhood-onset and adult-onset systemic lupus erythematosus. Arthritis and rheumatism. 2008 Feb:58(2):556-62. doi: 10.1002/art.23204. Epub
[PubMed PMID: 18240232]
[27]
Rodriguez-Ramirez S, Wiegley N, Mejia-Vilet JM. Kidney Biopsy in Management of Lupus Nephritis: A Case-Based Narrative Review. Kidney medicine. 2024 Feb:6(2):100772. doi: 10.1016/j.xkme.2023.100772. Epub 2023 Dec 6
[PubMed PMID: 38317756]
Level 3 (low-level) evidence
[28]
Yap DY, Chan TM. Lupus Nephritis in Asia: Clinical Features and Management. Kidney diseases (Basel, Switzerland). 2015 Sep:1(2):100-9. doi: 10.1159/000430458. Epub 2015 Aug 5
[PubMed PMID: 27536670]
[29]
Wang H, Ren YL, Chang J, Gu L, Sun LY. A Systematic Review and Meta-analysis of Prevalence of Biopsy-Proven Lupus Nephritis. Archives of rheumatology. 2018 Mar:33(1):17-25. doi: 10.5606/ArchRheumatol.2017.6127. Epub 2017 Jul 25
[PubMed PMID: 29900975]
Level 1 (high-level) evidence
[30]
Gasparotto M, Gatto M, Binda V, Doria A, Moroni G. Lupus nephritis: clinical presentations and outcomes in the 21st century. Rheumatology (Oxford, England). 2020 Dec 5:59(Suppl5):v39-v51. doi: 10.1093/rheumatology/keaa381. Epub
[PubMed PMID: 33280015]
[31]
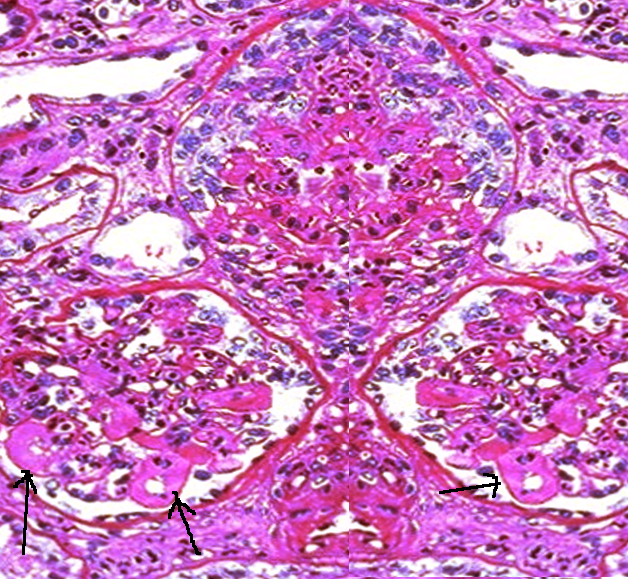
Hashmi AA, Ali J, Rahman M, Taseer AR, Kumar J, Irfan M. Spectrum of Morphologic Features of Lupus Nephritis According to Nephrology/Renal Pathology Society (ISN/RPS) Classification. Cureus. 2020 Sep 18:12(9):e10520. doi: 10.7759/cureus.10520. Epub 2020 Sep 18
[PubMed PMID: 33094061]
[32]
Sinicato NA, da Silva Cardoso PA, Appenzeller S. Risk factors in cardiovascular disease in systemic lupus erythematosus. Current cardiology reviews. 2013 Feb 1:9(1):15-9
[PubMed PMID: 23463953]
[33]
Bajema IM, Wilhelmus S, Alpers CE, Bruijn JA, Colvin RB, Cook HT, D'Agati VD, Ferrario F, Haas M, Jennette JC, Joh K, Nast CC, Noël LH, Rijnink EC, Roberts ISD, Seshan SV, Sethi S, Fogo AB. Revision of the International Society of Nephrology/Renal Pathology Society classification for lupus nephritis: clarification of definitions, and modified National Institutes of Health activity and chronicity indices. Kidney international. 2018 Apr:93(4):789-796. doi: 10.1016/j.kint.2017.11.023. Epub 2018 Feb 16
[PubMed PMID: 29459092]
[34]
Helget LN, Dillon DJ, Wolf B, Parks LP, Self SE, Bruner ET, Oates EE, Oates JC. Development of a lupus nephritis suboptimal response prediction tool using renal histopathological and clinical laboratory variables at the time of diagnosis. Lupus science & medicine. 2021 Aug:8(1):. doi: 10.1136/lupus-2021-000489. Epub
[PubMed PMID: 34429335]
[35]
Umeda R, Ogata S, Hara S, Takahashi K, Inaguma D, Hasegawa M, Yasuoka H, Yuzawa Y, Hayashi H, Tsuboi N. Comparison of the 2018 and 2003 International Society of Nephrology/Renal Pathology Society classification in terms of renal prognosis in patients of lupus nephritis: a retrospective cohort study. Arthritis research & therapy. 2020 Nov 4:22(1):260. doi: 10.1186/s13075-020-02358-x. Epub 2020 Nov 4
[PubMed PMID: 33148339]
Level 2 (mid-level) evidence
[36]
Li GM, Li YF, Zeng QQ, Zhang XM, Liu HM, Feng JY, Shi Y, Wu BB, Xu H, Sun L. Lupus podocytopathy and antiphospholipid syndrome in a child with SLE: A case report and literature review. Frontiers in pediatrics. 2022:10():950576. doi: 10.3389/fped.2022.950576. Epub 2022 Aug 19
[PubMed PMID: 36061375]
Level 3 (low-level) evidence
[37]
Mejia-Vilet JM, Zhang XL, Cruz C, Cano-Verduzco ML, Shapiro JP, Nagaraja HN, Morales-Buenrostro LE, Rovin BH. Urinary Soluble CD163: a Novel Noninvasive Biomarker of Activity for Lupus Nephritis. Journal of the American Society of Nephrology : JASN. 2020 Jun:31(6):1335-1347. doi: 10.1681/ASN.2019121285. Epub 2020 Apr 16
[PubMed PMID: 32300067]
[38]
Gupta R, Yadav A, Aggarwal A. Urinary soluble CD163 is a good biomarker for renal disease activity in lupus nephritis. Clinical rheumatology. 2021 Mar:40(3):941-948. doi: 10.1007/s10067-020-05343-6. Epub 2020 Aug 18
[PubMed PMID: 32809146]
[39]
Renaudineau Y, Chauveau D, Faguer S, Huart A, Ribes D, Pugnet G, Sailler L, Jamme T, Treiner E, Fortenfant F, Bost C, Carlé C, Belliere J. Urinary soluble CD163 is useful as "liquid biopsy" marker in lupus nephritis at both diagnosis and follow-up to predict impending flares. Journal of translational autoimmunity. 2024 Dec:9():100244. doi: 10.1016/j.jtauto.2024.100244. Epub 2024 Jun 20
[PubMed PMID: 39021518]
[40]
Malvar A, Pirruccio P, Alberton V, Lococo B, Recalde C, Fazini B, Nagaraja H, Indrakanti D, Rovin BH. Histologic versus clinical remission in proliferative lupus nephritis. Nephrology, dialysis, transplantation : official publication of the European Dialysis and Transplant Association - European Renal Association. 2017 Aug 1:32(8):1338-1344. doi: 10.1093/ndt/gfv296. Epub
[PubMed PMID: 26250434]
[41]
De Rosa M, Azzato F, Toblli JE, De Rosa G, Fuentes F, Nagaraja HN, Nash R, Rovin BH. A prospective observational cohort study highlights kidney biopsy findings of lupus nephritis patients in remission who flare following withdrawal of maintenance therapy. Kidney international. 2018 Oct:94(4):788-794. doi: 10.1016/j.kint.2018.05.021. Epub 2018 Jul 23
[PubMed PMID: 30045812]
[42]
Das U, Patel R, Guditi S, Taduri G. Correlation between the clinical remission and histological remission in repeat biopsy findings of quiescent proliferative lupus nephritis. Lupus. 2021 May:30(6):876-883. doi: 10.1177/0961203321995251. Epub 2021 Feb 20
[PubMed PMID: 33611965]
[43]
Malvar A, Alberton V, Lococo B, Lourenco M, Martinez J, Burna L, Besso C, Navarro J, Nagaraja HN, Khatiwada A, Wolf B, Rovin B. Remission of lupus nephritis: the trajectory of histological response in successfully treated patients. Lupus science & medicine. 2023 May:10(1):. doi: 10.1136/lupus-2023-000932. Epub
[PubMed PMID: 37258036]
[44]
Malvar A, Alberton V, Lococo B, Ferrari M, Delgado P, Nagaraja HN, Rovin BH. Kidney biopsy-based management of maintenance immunosuppression is safe and may ameliorate flare rate in lupus nephritis. Kidney international. 2020 Jan:97(1):156-162. doi: 10.1016/j.kint.2019.07.018. Epub 2019 Aug 20
[PubMed PMID: 31685314]
[45]
Fanouriakis A, Kostopoulou M, Cheema K, Anders HJ, Aringer M, Bajema I, Boletis J, Frangou E, Houssiau FA, Hollis J, Karras A, Marchiori F, Marks SD, Moroni G, Mosca M, Parodis I, Praga M, Schneider M, Smolen JS, Tesar V, Trachana M, van Vollenhoven RF, Voskuyl AE, Teng YKO, van Leew B, Bertsias G, Jayne D, Boumpas DT. 2019 Update of the Joint European League Against Rheumatism and European Renal Association-European Dialysis and Transplant Association (EULAR/ERA-EDTA) recommendations for the management of lupus nephritis. Annals of the rheumatic diseases. 2020 Jun:79(6):713-723. doi: 10.1136/annrheumdis-2020-216924. Epub 2020 Mar 27
[PubMed PMID: 32220834]
[46]
Plüß M, Piantoni S, Tampe B, Kim AHJ, Korsten P. Belimumab for systemic lupus erythematosus - Focus on lupus nephritis. Human vaccines & immunotherapeutics. 2022 Nov 30:18(5):2072143. doi: 10.1080/21645515.2022.2072143. Epub 2022 May 19
[PubMed PMID: 35588699]
[47]
Rúa-Figueroa Í, Salman-Monte TC, Pego Reigosa JM, Galindo Izquierdo M, Díez Álvarez E, Fernández-Nebro A, Román Ivorra JA, Calvo Penades I, Artaraz Beobide J, Calvo Alén J. Multidisciplinary consensus on the use of hydroxychloroquine in patients with systemic lupus erythematosus. Reumatologia clinica. 2024 Jun-Jul:20(6):312-319. doi: 10.1016/j.reumae.2024.03.002. Epub
[PubMed PMID: 38991825]
Level 3 (low-level) evidence
[48]
Carrión-Barberà I, Salman-Monte TC, Castell S, Castro F, Ojeda F, Carbonell J. Prevalence and factors associated with fatigue in female patients with systemic lupus erythematosus. Medicina clinica. 2018 Nov 9:151(9):353-358. doi: 10.1016/j.medcli.2017.12.007. Epub 2018 Feb 10
[PubMed PMID: 29439873]
[49]
Wirestam L, Enocsson H, Skogh T, Padyukov L, Jönsen A, Urowitz MB, Gladman DD, Romero-Diaz J, Bae SC, Fortin PR, Sanchez-Guerrero J, Clarke AE, Bernatsky S, Gordon C, Hanly JG, Wallace D, Isenberg DA, Rahman A, Merrill J, Ginzler E, Alarcón GS, Chatham WW, Petri M, Khamashta M, Aranow C, Mackay M, Dooley MA, Manzi S, Ramsey-Goldman R, Nived O, Steinsson K, Zoma A, Ruiz-Irastorza G, Lim S, Kalunian K, Inanc M, van Vollenhoven R, Ramos-Casals M, Kamen DL, Jacobsen S, Peschken C, Askanase A, Stoll T, Bruce IN, Wetterö J, Sjöwall C. Osteopontin and Disease Activity in Patients with Recent-onset Systemic Lupus Erythematosus: Results from the SLICC Inception Cohort. The Journal of rheumatology. 2019 May:46(5):492-500. doi: 10.3899/jrheum.180713. Epub 2019 Jan 15
[PubMed PMID: 30647177]
[50]
Tsai WT, Chang HC, Wang CT, Chiang BL, Lin YT. Long-term outcomes in lupus patients receiving different renal replacement therapy. Journal of microbiology, immunology, and infection = Wei mian yu gan ran za zhi. 2019 Aug:52(4):648-653. doi: 10.1016/j.jmii.2018.12.010. Epub 2019 Jan 4
[PubMed PMID: 30642809]
[51]
Ruiz-Irastorza G, Dueña-Bartolome L, Dunder S, Varona J, Gomez-Carballo C, Dominguez-Cainzos J, Rodrigo-Manjon A, Bueno L, Richez C, Duffau P, Blanco P, Lazaro E. Eurolupus cyclophosphamide plus repeated pulses of methyl-prednisolone for the induction therapy of class III, IV and V lupus nephritis. Autoimmunity reviews. 2021 Oct:20(10):102898. doi: 10.1016/j.autrev.2021.102898. Epub 2021 Jul 15
[PubMed PMID: 34274543]
[52]
Portalatin GM, Gebreselassie SK, Bobart SA. Lupus nephritis - An update on disparities affecting african americans. Journal of the National Medical Association. 2022 Jun:114(3S2):S34-S42. doi: 10.1016/j.jnma.2022.05.005. Epub 2022 May 18
[PubMed PMID: 35595581]
[53]
Zhang H, Zhou M, Han X, Yang Y, Yu X. Mycophenolate mofetil in the treatment of Chinese patients with lupus nephritis: A PRISMA-compliant meta-analysis. Medicine. 2020 Aug 14:99(33):e21121. doi: 10.1097/MD.0000000000021121. Epub
[PubMed PMID: 32871981]
Level 1 (high-level) evidence
[54]
Jiang N, Li M, Zhang H, Duan X, Li X, Fang Y, Li H, Yang P, Luo H, Wang Y, Peng L, Zhao J, Wu C, Wang Q, Tian X, Zhao Y, Zeng X. Sirolimus versus tacrolimus for systemic lupus erythematosus treatment: results from a real-world CSTAR cohort study. Lupus science & medicine. 2022 Jan:9(1):. doi: 10.1136/lupus-2021-000617. Epub
[PubMed PMID: 34980680]
[55]
Dooley MA, Jayne D, Ginzler EM, Isenberg D, Olsen NJ, Wofsy D, Eitner F, Appel GB, Contreras G, Lisk L, Solomons N, ALMS Group. Mycophenolate versus azathioprine as maintenance therapy for lupus nephritis. The New England journal of medicine. 2011 Nov 17:365(20):1886-95. doi: 10.1056/NEJMoa1014460. Epub
[PubMed PMID: 22087680]
[56]
Ordi-Ros J, Sáez-Comet L, Pérez-Conesa M, Vidal X, Mitjavila F, Castro Salomó A, Cuquet Pedragosa J, Ortiz-Santamaria V, Mauri Plana M, Cortés-Hernández J. Enteric-coated mycophenolate sodium versus azathioprine in patients with active systemic lupus erythematosus: a randomised clinical trial. Annals of the rheumatic diseases. 2017 Sep:76(9):1575-1582. doi: 10.1136/annrheumdis-2016-210882. Epub 2017 Apr 27
[PubMed PMID: 28450313]
Level 1 (high-level) evidence
[57]
Rovin BH, Furie R, Latinis K, Looney RJ, Fervenza FC, Sanchez-Guerrero J, Maciuca R, Zhang D, Garg JP, Brunetta P, Appel G, LUNAR Investigator Group. Efficacy and safety of rituximab in patients with active proliferative lupus nephritis: the Lupus Nephritis Assessment with Rituximab study. Arthritis and rheumatism. 2012 Apr:64(4):1215-26. doi: 10.1002/art.34359. Epub 2012 Jan 9
[PubMed PMID: 22231479]
[58]
Jorge A, Wallace ZS, Lu N, Zhang Y, Choi HK. Renal Transplantation and Survival Among Patients With Lupus Nephritis: A Cohort Study. Annals of internal medicine. 2019 Feb 19:170(4):240-247. doi: 10.7326/M18-1570. Epub 2019 Jan 22
[PubMed PMID: 30665236]
[59]
Sammaritano LR, Bermas BL, Chakravarty EE, Chambers C, Clowse MEB, Lockshin MD, Marder W, Guyatt G, Branch DW, Buyon J, Christopher-Stine L, Crow-Hercher R, Cush J, Druzin M, Kavanaugh A, Laskin CA, Plante L, Salmon J, Simard J, Somers EC, Steen V, Tedeschi SK, Vinet E, White CW, Yazdany J, Barbhaiya M, Bettendorf B, Eudy A, Jayatilleke A, Shah AA, Sullivan N, Tarter LL, Birru Talabi M, Turgunbaev M, Turner A, D'Anci KE. 2020 American College of Rheumatology Guideline for the Management of Reproductive Health in Rheumatic and Musculoskeletal Diseases. Arthritis & rheumatology (Hoboken, N.J.). 2020 Apr:72(4):529-556. doi: 10.1002/art.41191. Epub 2020 Feb 23
[PubMed PMID: 32090480]
[60]
Wahl DG, Bounameaux H, de Moerloose P, Sarasin FP. Prophylactic antithrombotic therapy for patients with systemic lupus erythematosus with or without antiphospholipid antibodies: do the benefits outweigh the risks? A decision analysis. Archives of internal medicine. 2000 Jul 10:160(13):2042-8
[PubMed PMID: 10888978]
[61]
Athanassiou P, Athanassiou L. Current Treatment Approach, Emerging Therapies and New Horizons in Systemic Lupus Erythematosus. Life (Basel, Switzerland). 2023 Jul 1:13(7):. doi: 10.3390/life13071496. Epub 2023 Jul 1
[PubMed PMID: 37511872]
[62]
Urbanus RT, Siegerink B, Roest M, Rosendaal FR, de Groot PG, Algra A. Antiphospholipid antibodies and risk of myocardial infarction and ischaemic stroke in young women in the RATIO study: a case-control study. The Lancet. Neurology. 2009 Nov:8(11):998-1005. doi: 10.1016/S1474-4422(09)70239-X. Epub 2009 Sep 25
[PubMed PMID: 19783216]
Level 2 (mid-level) evidence
[63]
Furie R, Rovin BH, Houssiau F, Malvar A, Teng YKO, Contreras G, Amoura Z, Yu X, Mok CC, Santiago MB, Saxena A, Green Y, Ji B, Kleoudis C, Burriss SW, Barnett C, Roth DA. Two-Year, Randomized, Controlled Trial of Belimumab in Lupus Nephritis. The New England journal of medicine. 2020 Sep 17:383(12):1117-1128. doi: 10.1056/NEJMoa2001180. Epub
[PubMed PMID: 32937045]
Level 1 (high-level) evidence
[64]
Shipa M, Embleton-Thirsk A, Parvaz M, Santos LR, Muller P, Chowdhury K, Isenberg DA, Doré CJ, Gordon C, Ehrenstein MR, BEAT-LUPUS Investigators. Effectiveness of Belimumab After Rituximab in Systemic Lupus Erythematosus : A Randomized Controlled Trial. Annals of internal medicine. 2021 Dec:174(12):1647-1657. doi: 10.7326/M21-2078. Epub 2021 Oct 26
[PubMed PMID: 34698499]
Level 1 (high-level) evidence
[65]
Saxena A, Ginzler EM, Gibson K, Satirapoj B, Santillán AEZ, Levchenko O, Navarra S, Atsumi T, Yasuda S, Chavez-Perez NN, Arriens C, Parikh SV, Caster DJ, Birardi V, Randhawa S, Lisk L, Huizinga RB, Teng YKO. Safety and Efficacy of Long-Term Voclosporin Treatment for Lupus Nephritis in the Phase 3 AURORA 2 Clinical Trial. Arthritis & rheumatology (Hoboken, N.J.). 2024 Jan:76(1):59-67. doi: 10.1002/art.42657. Epub 2023 Sep 15
[PubMed PMID: 37466424]
Level 1 (high-level) evidence
[66]
Xipell M, Lledó GM, Egan AC, Tamirou F, Del Castillo CS, Rovira J, Gómez-Puerta JA, García-Herrera A, Cervera R, Kronbichler A, Jayne DRW, Anders HJ, Houssiau F, Espinosa G, Quintana LF. From systemic lupus erythematosus to lupus nephritis: The evolving road to targeted therapies. Autoimmunity reviews. 2023 Oct:22(10):103404. doi: 10.1016/j.autrev.2023.103404. Epub 2023 Aug 3
[PubMed PMID: 37543287]
[67]
Malvar A, Alberton V, Recalde C, Heguilen R. Repeat kidney biopsy findings of lupus nephritis patients in clinical remission treated with Mycophenolate associated with Belimumab or Mycophenolate plus standard of care therapy. A "post-hoc" analysis of participants in the BLISS-LN and open label extension study belonging to a single center. Lupus. 2023 Oct:32(12):1394-1401. doi: 10.1177/09612033231204070. Epub 2023 Sep 27
[PubMed PMID: 37754750]
[68]
Mejia-Vilet JM, Turner-Stokes T, Houssiau F, Rovin BH. Kidney involvement in systemic lupus erythematosus: From the patient assessment to a tailored treatment. Best practice & research. Clinical rheumatology. 2023 Dec:37(4):101925. doi: 10.1016/j.berh.2023.101925. Epub 2023 Dec 26
[PubMed PMID: 38151362]
[69]
Davies R, Peng SL, Lickliter J, McLendon K, Enstrom A, Chunyk AG, Blanchfield L, Wang N, Blair T, Thomas HM, Smith A, Dillon SR. A first-in-human, randomized study of the safety, pharmacokinetics and pharmacodynamics of povetacicept, an enhanced dual BAFF/APRIL antagonist, in healthy adults. Clinical and translational science. 2024 Nov:17(11):e70055. doi: 10.1111/cts.70055. Epub
[PubMed PMID: 39494621]
Level 1 (high-level) evidence
[70]
Jorge A, Wallace ZS, Zhang Y, Lu N, Costenbader KH, Choi HK. All-Cause and Cause-Specific Mortality Trends of End-Stage Renal Disease Due to Lupus Nephritis From 1995 to 2014. Arthritis & rheumatology (Hoboken, N.J.). 2019 Mar:71(3):403-410. doi: 10.1002/art.40729. Epub 2019 Jan 9
[PubMed PMID: 30225916]