Continuing Education Activity
Adamantinomas are rare, low-grade malignant bone tumors primarily observed in individuals aged 20 to 40. Adamantinomas have a mortality rate of 6% to 18% and a metastasis frequency of 12% to 29% due to their local aggressiveness and metastatic potential. Timely diagnosis and treatment are crucial in mitigating this condition's associated morbidity and mortality risks. The unpredictable behavior of adamantinomas, including late recurrences after surgical excision, underscores the necessity for long-term, vigilant follow-up care. This activity elucidates the clinical characteristics, diagnostic evaluation, and treatment options for adamantinomas, emphasizing the importance of collaboration among healthcare professionals. This activity also aims to enhance the clinical competency of interprofessional healthcare team members, including orthopedic surgeons, oncologists, radiologists, pathologists, and nurses involved in caring for patients with adamantinomas. Upon completing the activity, participants can identify clinical presentations, apply suitable diagnostic techniques, assess treatment choices, and understand the significance of sustained follow-up care and interprofessional teamwork.
Objectives:
Identify adamantinoma's clinical and radiological presentations and distinguish them from other bone tumors or lesions.
Differentiate among different histological patterns of adamantinoma and its variants, such as differentiated and osteofibrous dysplasia-like adamantinomas.
Apply the current guidelines and best practices in managing adamantinomas, considering individual patient factors, tumor characteristics, and available treatment modalities to optimize patient care.
Collaborate within interprofessional healthcare teams, including oncologists, orthopedic surgeons, radiologists, pathologists, and nurses, to ensure comprehensive and coordinated patient care.
Introduction
Adamantinomas are rare, low-grade malignant bone tumors of uncertain histogenesis that predominately affect the diaphyses and metaphyses of the tibia. The tumor is called adamantinoma due to its histological similarity to ameloblastoma, often found in the mandible.[1] Histopathologically, adamantinoma displays biphasic patterns consisting of epithelial cells and osteofibrous components.
There are 2 types of adamantinomas—classical and differentiated—and the latter resembles osteofibrous dysplasia.[2] Despite advancements in imaging techniques, the definitive diagnosis of adamantinoma primarily relies on histopathological examination.
Etiology
Currently, the origin of adamantinoma remains unknown. A traditionally accepted pathogenesis theory suggests the early displacement of basal epithelial cells of the skin during embryological development.[3] This theory is supported by the fact that the most common site of adamantinoma is the anterior tibia, where the enchondral bone formation is closest to the skin surface.
Immunohistochemical and ultrastructural investigations have yielded some evidence suggesting that adamantinoma might have an epithelial origin.[3] However, the connection between adamantinoma and osteofibrous dysplasia is still debatable. The possible association between these 2 conditions holds significance for the diagnosis, prognosis, and treatment of patients with adamantinoma.[4]
Epidemiology
Adamantinoma is an infrequent tumor, accounting for approximately 0.4% of all primary malignant bone tumors. This tumor exhibits a slight male predominance, with a 5:4 male-to-female ratio. Adamantinomas predominantly affect individuals aged 20 to 40, whereas they are rare in pediatric and older populations.
Although adamantinomas most commonly affect the anterior metaphysis or diaphysis of the tibia, they can also impact other body areas, including the fibula, ulna, femur, humerus, and radius.[2][5]
Pathophysiology
A consistent pattern of numerical abnormalities has been observed in classic and osteofibrous dysplasia-like adamantinomas, characterized by additional copies of chromosomes 7, 8, 12, 19, and 21.[6][7]
Histopathology
Macroscopic Findings
Classic adamantinomas usually present as cortical tumors, which are well-defined and have a yellowish-gray appearance. These tumors exhibit a lobulated structure with a firm-to-bony consistency and are often accompanied by peripheral sclerosis. The tumors may manifest as either a single lesion or, occasionally, as multiple lesions. Macroscopically, observable cystic spaces within the tumor are commonly filled with straw-colored or blood-like fluid.[3]
Histological Findings
Classical adamantinomas are characterized by distinct epithelial and osteofibrous components that can be mixed in various proportions and differentiation patterns. The 4 primary differentiation patterns observed in classic adamantinoma are basaloid, tubular, spindle cell, and squamous.[8]
Although all 4 patterns of classic adamantinoma may coexist, the basaloid and tubular patterns are the most frequently observed. The spindle-cell component is often encountered in recurrences, lining cystic spaces, and metastases. The osteofibrous component comprises spindle cells arranged in a storiform pattern, typically accompanied by woven bone trabeculae within or near the center of the lesion. Osteoblasts prominently encircle these trabeculae and exhibit varying degrees of transformation to lamellar bone at the tumor's periphery.[9]
Foam cells or myxoid change may be present, and mast cells or multinucleated giant cells are occasionally detected. Mitotic activity within the tumor is usually low. A fifth histological pattern, the osteofibrous dysplasia-like variant, is characterized by the predominance of osteofibrous tissue. In this variant, small clusters of epithelial cells are detectable only with careful examination or through immunohistochemistry.[10]
Extensive sampling of adamantinoma is significant, especially in the differentiated form where the epithelial component is encountered only in focal areas.
Immunohistochemical Study
In adamantinoma, the fibrous tissue component tests positive for vimentin, whereas the epithelial cells show coexpression of keratin, epithelial membrane antigen (EMA), vimentin, p63, and podoplanin.[11][12] Estrogen, progesterone, and N-cadherin are present in classic adamantinoma but not in osteofibrous dysplasia-like adamantinoma.[13]
In classic adamantinomas, the epithelial component is surrounded by a continuous basement membrane consisting of collagen IV, laminin, and galectin 3.[13] However, there may be multiple interruptions or the absence of a surrounding basement membrane in less distinct epithelial islands. Expression of epidermal growth factor (EGF) and epidermal growth factor receptor (EGFR) is confined to the epithelial component. On the other hand, fibroblast growth factor 2 (FGF2) and fibroblast growth factor receptor 1 (FGFR1) are detected in both components. In culture, adamantinoma cells also express macrophage colony-stimulating factor (M-CSF) and receptor activator of nuclear factor kappa-B ligand (RANKL), possibly contributing to the osteolysis observed.[14][15]
History and Physical
Adamantinomas typically exhibit a prolonged clinical course characterized by gradual and progressive growth. The primary concern reported by patients is the presence of a slow-growing swelling, which may or may not be accompanied by pain.[16] Bone deformities and the risk of pathological fractures can also arise, prompting patients to seek medical attention. In addition, some patients may exhibit neurological deficits in cases where the spine is affected.[3] Notably, as many as 23% of patients with adamantinoma may experience pathological fractures.[17]
The disease may remain inconspicuous in the early stages because of subtle symptoms and gradual progression. Patients often tolerate symptoms for several years before seeking medical help, contributing to delays in diagnosis and treatment.
Evaluation
Plain Radiograph
On x-ray, adamantinoma typically appears as a well-circumscribed, cortical tumor with a multilobulated, osteolytic pattern. Intralesional opacities, septation, and peripheral sclerosis may also be seen. Multifocality within the same bone is regularly observed. These multifocal radiolucencies, surrounded by ring-shaped densities, produce the characteristic ''soap-bubble'' appearance.[18]
The lesion is typically confined within the intracortical region and extends longitudinally along the bone. However, in some cases, it can result in cortical destruction and invade the medullary cavity or adjacent periosteum and soft tissues. In such cases, a lamellar or solid periosteal reaction is typically associated with the .lesion.[18]
Computed Tomography Scan
A computed tomography (CT) scan effectively visualizes the soft tissue extension and cortical involvement of adamantinomas. However, a CT scan does not provide detailed imaging of the intraosseous extension of these tumors. CT scans are integral to the standard diagnostic evaluation of adamantinomas and can aid in detecting pulmonary metastases.[3]
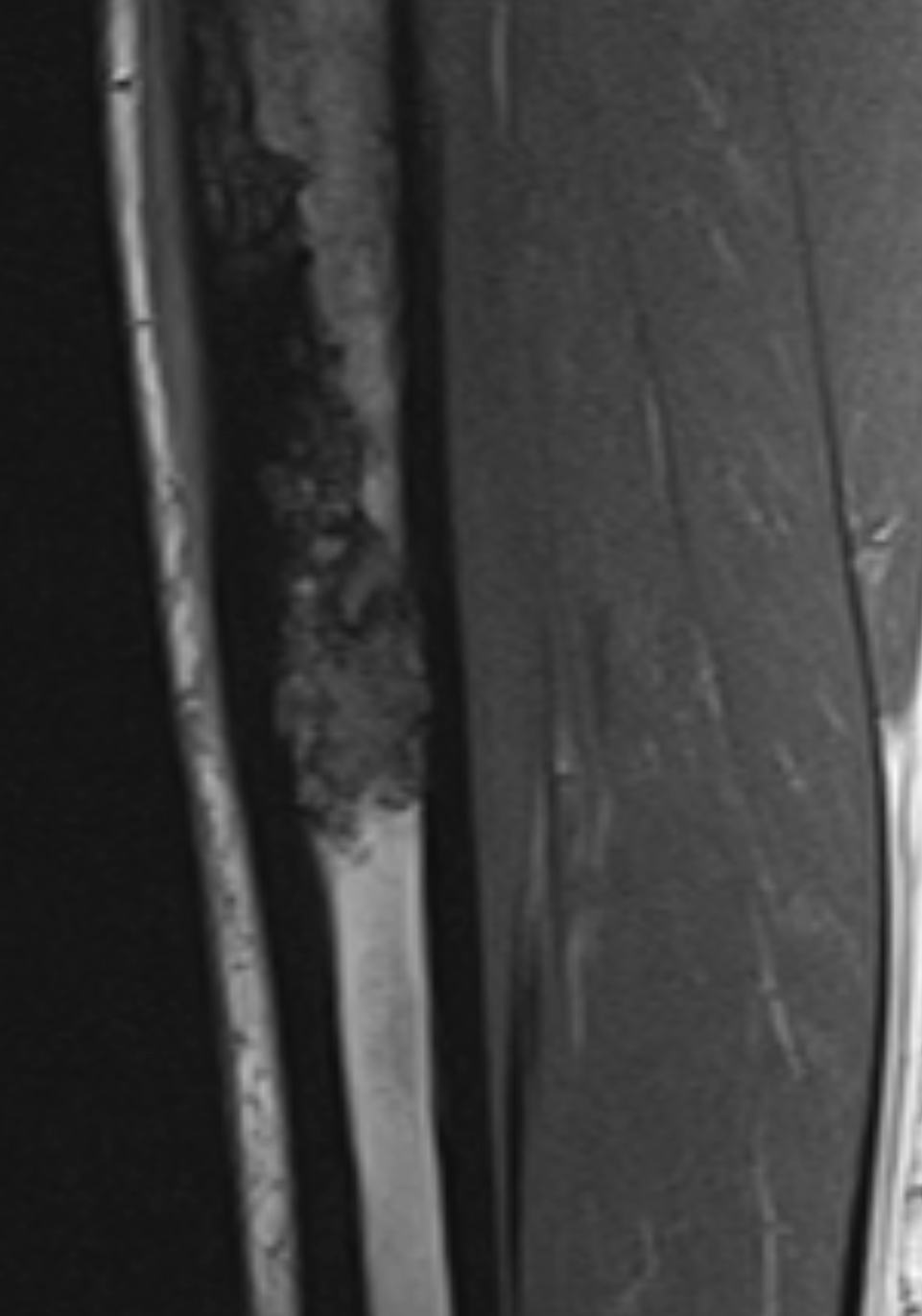
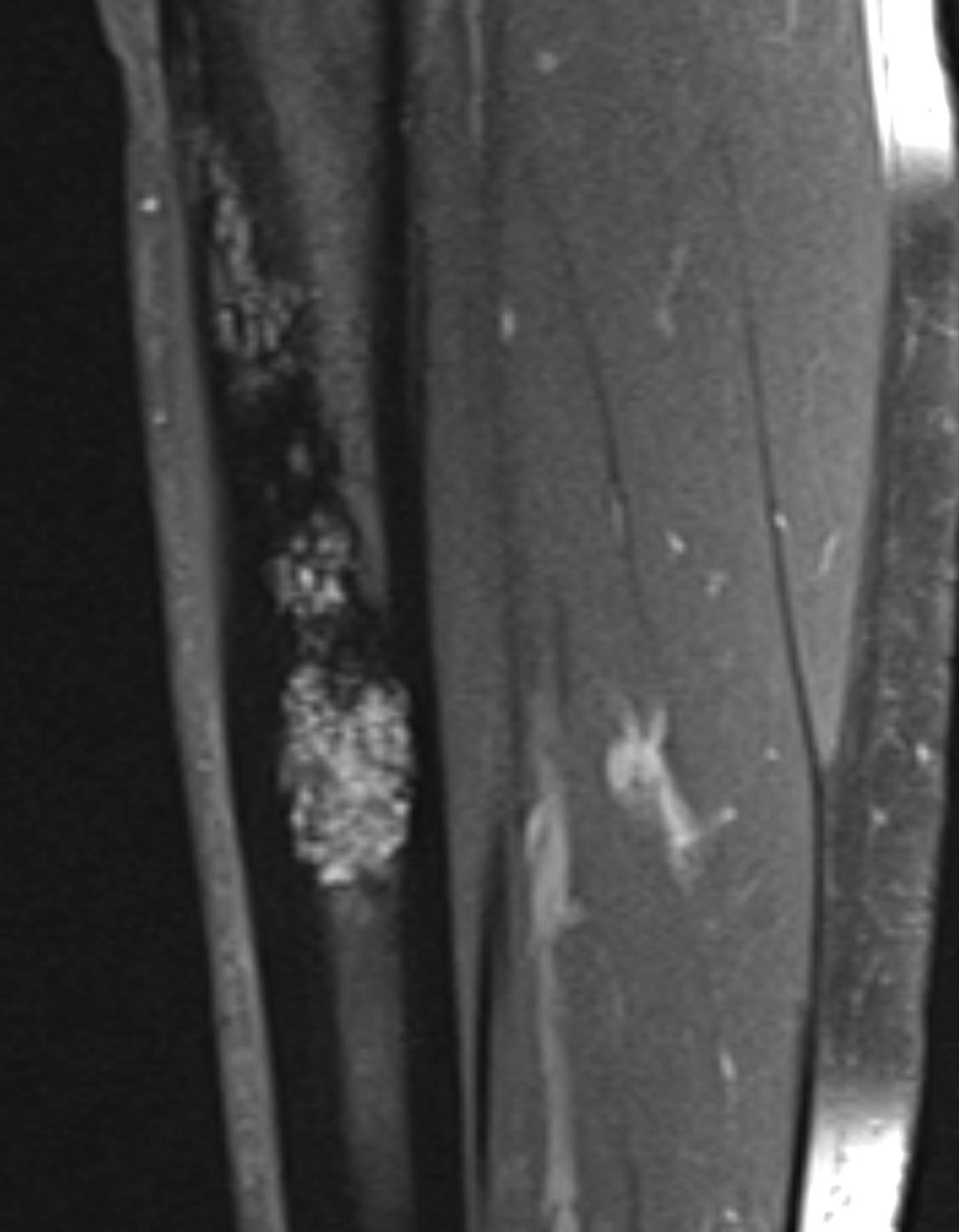
Magnetic Resonance Imaging
Magnetic resonance imaging (MRI) is crucial in the locoregional staging of adamantinomas, as it provides detailed visualization of distant cortical foci, intramedullary involvement, and soft tissue extension. MRI is also a valuable tool for determining tumor-free margins, a critical aspect of surgical planning to ensure complete tumor removal. MRI aids in evaluating the extent of the disease and assists in determining the appropriate strategy for reconstructive surgery if required.[19]
MRI reveals the following 2 morphological patterns of adamantinoma:
- Multiple small nodules in 1 or more foci
- A solitary lobulated focus
Adamantinomas typically exhibit low signal intensity on T1-weighted images and high signal intensity on T2-weighted images. However, it is noteworthy that these findings are nonspecific and can be seen in various other conditions.[3][19]
Treatment / Management
Due to its rarity, no clear consensus or standardized recommendations for managing adamantinomas are documented in the literature.[20] The initial course of adamantinoma treatment is crucial and necessitates a careful biopsy while avoiding curettage. Curettage is associated with an increased risk of recurrence,[8] and the recurrence rate in typical adamantinoma after intralesional curettage may reach as high as 90%.[21]
The local recurrence rate of these adamantinoma tumors after marginal excision is up to 32%.[22] Patients who underwent resection in one study had a 29% local recurrence rate, whereas those with curettage experienced a 100% local recurrence rate. Considering these findings, Puchner et al strongly recommended wide resections as the preferred approach for managing adamantinoma.[23]
Resection
The initial step in treating adamantinoma involves the resection of the bone tumor through en bloc removal with wide-margin excision. After tumor removal, the subsequent step involves reconstructing the resulting bony defect. Various techniques can be utilized to fill the excised bone defect, including distraction osteogenesis, intercalary allografts, vascularized autografts, and tailored prostheses or endoprosthesis.[3][24]
The most effective treatment for adamantinoma is wide excision with clear margins.[7][25] According to a study conducted by Qureshi et al, 87.2% of patients who underwent limb salvage resection survived for 10 years. Out of 70 patients, 50 could preserve their limbs, resulting in a limb preservation proportion of 84%. Nonetheless, the study reported a high frequency of limb reconstruction-related problems.[17] Qureshi further explained that wide surgical margins were associated with a decreased risk of local recurrence compared to marginal or intralesional margins (P < .00005).
Recurrence of Adamantinoma
The behavior of adamantinoma is known to be relatively unpredictable to a significant extent. In a cohort study by Schutgens et al, 27% of patients experienced a local recurrence of adamantinoma after more than 10 years of follow-up. Furthermore, adamantinoma can metastasize to other parts of the body, including the lungs, nearby lymph nodes, and the spine.[26] According to the literature, local recurrences and metastases have been reported to occur up to 36 years after initial diagnosis due to their slow-growing nature. Therefore, individuals should monitor for any changes.[25][27]
As a result, individuals diagnosed with adamantinoma should undergo long-term observation, often extending beyond 15 years.[28][29][30] Regular monitoring should include lung imaging, typically performed annually or in the event of a local recurrence, and physical examinations to check for lymphadenopathy. Surgical resection is recommended for treating metastatic lesions and recurrences identified during regular monitoring.[31]
Matastasectomy of Pulmonary Recurrences
Metastasectomy is considered the first-line therapy for pulmonary recurrences. According to a Dutch study, both radiation treatment and chemotherapy did not significantly impact tumor volume or survival.[29] Radiotherapy and chemotherapy have shown limited effectiveness in the treatment of adamantinoma.[32] There is only 1 reported case in the literature where a patient achieved stable health 4 years after undergoing numerous chemotherapy regimens and radiation therapy cycles.[33]
Radiation Therapy
Although radiation treatment is generally ineffective in directly treating adamantinoma, it can relieve back pain and potentially reduce the need for opioid analgesics. Moreover, some patients have demonstrated sustained results with targeted treatment using tyrosine kinase inhibitors.[34][35]
Amputation
Amputation may be deemed necessary for adamantinoma if there is a local recurrence or if en bloc resection and limb salvage are not viable options. Notably, there is no significant difference between limb salvage and amputation in survival rate.[7] Because of the high rate of recurrence, curettage is not recommended.[5]
Differential Diagnosis
According to several authors, a significant association exists between differentiated adamantinoma or osteofibrous dysplasia-like adamantinoma and osteofibrous dysplasia. This connection can pose challenges in differential diagnosis due to similar histological and radiological characteristics, as well as their typical location in the tibia.[23] From a clinical, radiological, and histological perspective, adamantinoma can resemble various bone tumors, including bone cysts, giant cell tumors, and malignant tumors such as chondrosarcoma, angiosarcoma, and metastases.[3]
Prognosis
Adamantinoma is a locally aggressive neoplasm with the potential for metastasis. In cases of inadequate surgical treatment, the tumor frequently recurs.
Risk factors for recurrent or metastatic disease include the following:[36]
- Symptoms lasting for less than 5 years
- Male gender
- Patients younger than 20
- Pain upon presentation
- Initial treatment involving curettage or resection
- Absence of squamous differentiation within the tumor
- An increase in the epithelium-to-stroma ratio
Adamantinomas can potentially metastasize in approximately 15% to 30% of cases, typically through hematogenous or lymphatic routes. Common sites of metastasis include the lungs, lymph nodes, bones, and abdominal viscera.[3] According to the epidemiological study conducted by Aytekin et al, the survival rates for adamantinoma at 5 and 10 years were reported as 98.8% and 91.5%, respectively. Furthermore, the study demonstrated that survival time remained unaffected by sex, chronological age, ethnicity, marital status, tumor site, or year of detection.[37] In another study conducted by Houdek et al over a period of 16 years, 46 patients showed a 33% recurrence rate.[16]
Complications
According to the literature, the adamantinoma recurrence rate can range from 30% to 35%.[36] The mortality rate associated with adamantinoma ranges from 6% to 18%.[17] Metastasis to the lung or lymph nodes can occur in 12% to 29% of cases.[17]
Consultations
Orthopedics and oncology specialists, including those listed below, should be consulted for adamantinoma evaluation.
Orthopedics: Orthopedic surgeons play a significant role in the diagnosis, surgical management, and reconstruction of bone tumors, including adamantinoma.
Oncology: Oncologists specializing in medical or radiation oncology provide their expertise in systemic treatment and adjuvant therapies for adamantinoma.
Surgical oncology: Surgical oncologists are involved in the comprehensive surgical management and coordination of treatment strategies for patients with adamantinoma.
Deterrence and Patient Education
Patient education is a crucial component of adamantinoma management. When offering education to patients, healthcare providers need to address the below-mentioned key points.
Explanation of the condition: The primary responsibility of healthcare providers is to provide a clear and concise description of adamantinoma to patients, highlighting its rarity and aggressive nature as a bone tumor. In addition, they should inform the patients about the primary location of adamantinoma in the bones, such as the anterior tibia, emphasizing its locally invasive behavior.
Symptoms and metastasis: When educating patients, healthcare providers should discuss typical symptoms with them, which may include a slow-growing swelling with or without pain. Furthermore, patients should be informed that adamantinoma has the potential to metastasize to the lungs or lymph nodes in approximately 15% to 30% of cases.
Recurrence: The high recurrence rate of adamantinoma should be highlighted, which is approximately 33% even after excision. Healthcare providers should emphasize the importance of long-term follow-up care and patient monitoring for early recurrence detection.
Patience and time frame: Healthcare professionals should set realistic expectations with patients by explaining that recovery from adamantinoma takes time. In discussions with patients, potential options for reconstructive procedures after tumor excision should be explored to restore both function and aesthetics.
Mental health: Emphasizing the significance of mental health, offering support to patients and their family members through counseling, and highlighting the availability of resources to address their emotional well-being are crucial components of effective treatment. Healthcare providers should counsel patients that feeling depressed or anxious is a common psychological response to being diagnosed with adamantinoma.
Enhancing Healthcare Team Outcomes
A multidisciplinary team of experts from various medical fields, including orthopedics, pathology, medical and surgical oncology, and imaging, is necessary for optimal care of patients with adamantinoma. The combined expertise of the specialists is indispensable for ensuring accurate diagnosis, prognosis, and comprehensive management of the condition in patients. Involving musculoskeletal radiologists and pathologists in interpreting imaging results and tissue samples is crucial for establishing a definitive diagnosis and determining the most appropriate course of action.
As pain management is significant for the care of adamantinoma patients, engaging a pain expert in the treatment process can help alleviate discomfort and improve their quality of life. Due to the common occurrence of depression and anxiety in patients with adamantinoma, engaging a mental health nurse to counsel patients and their family members is advisable.
Nurses in the oncology department play a vital role in care coordination, follow-up, and patient education. They should inform the patient and their family about the available treatment options, techniques for pain management, and the support services accessible to them. For patients in advanced stages of adamantinoma, including a palliative care team is crucial. This specialized team provides care focused on symptom management and improves patients' overall well-being.
Orthopedic oncologists are critical in developing and implementing a comprehensive treatment strategy for patients, including removing the adamantinoma tumor and performing any necessary reconstructive procedures. Their expertise is crucial in accurately diagnosing the condition and selecting the most appropriate therapeutic approach, considering factors such as gross, radiographic, and microscopic findings.
Due to the potential for extraosseous metastases and tumor recurrence, long-term monitoring of patients is essential after therapy. An interprofessional team approach is necessary to enhance patient outcomes and improve their quality of life.