Continuing Education Activity
Uric acid renal calculi are formed as a consequence of various metabolic abnormalities. Although rare, its prevalence is increasing with the change in the lifestyle of people. This activity illustrates the evaluation and management of uric acid Renal calculi and highlights the role of the interprofessional team in improving care for patients with this condition.
Objectives:
- Identify the etiology of uric acid stones in the renal system.
- Review pathophysiology of the formation of uric acid stones.
- Outline the management options available for uric acid stones.
Introduction
Uric acid, a heterocyclic compound, is produced as a byproduct of purine metabolism. It can be generated from endogenous as well as exogenous sources. The human body makes about 300 - 400 mg of uric acid per day, with most of it being produced in the liver. Purines degenerate into inosine and hypoxanthine. Hypoxanthine is further metabolized into xanthine and uric acid in the presence of xanthine oxidase enzyme. In most mammals, uric acid is transformed to allantoin by enzymatic activity of uricase. Allantoin, being a very soluble chemical, does not create any pathology. However, in humans, this enzyme is nonfunctional, so the end product of purine metabolism is uric acid, a weak acid that is relatively insoluble. Thus, high levels of uric acid in the urine and serum can lead to its deposition in joints and kidneys, leading to gout and nephrolithiasis. Exogenous sources include meat, fish, alcohol, sweet drinks, sweetbreads, and organ meats which are particularly high in purines.
The organs responsible for the elimination and excretion of uric acid are the kidneys and intestines. In the intestinal tract, uric acid is transformed into ammonia and carbon dioxide. Bacteria utilize the intestinal ammonia for metabolism. In the kidneys, almost 100% of uric acid is filtered by glomerulus. Uric acid is further reabsorbed, secreted, and reabsorbed in the proximal convoluted tubule (PCT), ultimately resulting in only 10% fractional elimination in the urine.
Uric acid was first isolated by a Swedish pharmacist Scheele in 1776. Fourcroy examined about 600 stones from 1736 to 1802 and also suggested the term uric acid.[1][2][3][4]
Etiology
Uric acid calculi are predominantly caused by highly acidic urine, excessive urinary uric acid and relative dehydration, but they have a multifactorial etiology with multiple determinants as well which are outlined below:
- Idiopathic uric acid lithiasis (gouty diathesis) encompasses people who have no identifiable cause for uric acid stone formation. The biochemical profiling of such people typically shows a low urine pH accompanied by a very low fractional excretion of urate (little urine uric acid in the presence of a significantly elevated serum uric acid). These findings are very similar to primary gout. Thus idiopathic uric acid lithiasis is assumed to be an underlying abnormality of primary gout. [5]
- Approximately 10% to 20% of patients with primary gout produce uric acid nephrolithiasis. The biochemical profile of these patients is similar to idiopathic patients, including low urine pH and low excretion of uric acid. The mechanism responsible for high levels of uric acid in these patients is reduced uric acid urinary excretion. Consumption of alcohol, a high fructose diet, and high animal protein diet can increase the risk of gout and uric acid stones. Low urine pH is also one of the significant contributing factors.
- People with metabolic syndrome are predisposed to the formation of uric acid stones. Metabolic syndrome comprises diabetes, high waist circumference, and high cholesterol levels due to insulin resistance. There is an inverse correlation between the pH of the urine and body weight. The entity responsible for the low urinary pH is a deficit in buffering of urinary acid by ammonium due to impaired renal NH4+ production.
- People with inflammatory bowel disorders like Crohn disease and people who have ileostomies are at considerable risk for uric acid stone formation. They experience chronic diarrhea, which can lead to loss of fluid and bicarbonate ions, producing low urine volume (hypovolemia) and systemic metabolic acidosis.
- Genetic disorders that lead to hyperuricemia, including X linked recessive Lesch-Nyhan syndrome and Type 1 collagen storage disorder, are also etiological causes. Renal disorders, including Hartnup disease, Wilson's disease, and familial hypouricemic hyperuricosuria, can also lead to increased urinary uric acid excretion.
- Acquired causes include diet, malignancy, lymphoproliferative disorders, and drugs that compete with uric acid in the kidneys. These drugs lessen uric acid reabsorption, adding to increased urinary uric acid and renal stone formation. Patients with malignancy exhibit high levels of uric acid due to the rapid cell turnover. They are particularly predisposed to uric acid stone formation when they are on chemotherapy due to tumor cell necrosis. [1][4]
Epidemiology
Uric acid stones account for about 10% of all renal calculi in the United States. However, the incidence and prevalence of these stones around the world varies depending upon ethnicity and geography. More than 50% of the stones among Hmong immigrants in the United States are uric acid stones. Uric acid calculi account for about 57% of stones in Sudan and 75% in Israel. The prevalence ranges depending upon the sex of the patient, with a higher occurrence rate among women. People with type 2 diabetes mellitus, metabolic syndrome, and obesity are at a substantially higher risk of developing uric acid stones than the general population.
The environment also plays a role in nephrolithiasis risk. A study done in Saudi Arabia found increased episodes of renal colic with a raised temperature. The nephrolithiasis formation rate is also higher among workers in factories with hot surroundings. Both of these findings suggest that dehydration significantly contributes to uric acid stone disease.
A recent study comparing the existence of nephrolithiasis among developed and developing nations showed an overall increase in the incidence as well as the prevalence of renal lithiasis. This increase in stone disease is especially notable in developing countries because of the shift in the socio-economic condition of the population. As the population becomes more affluent, they tend to adopt a more Western diet with more animal protein in their food which increases their tendency to produce uric acid. Global warming is also considered a contributing factor. The review also identified an increased production of uric acid stones among developing countries as opposed to industrialized nations. However, data from the developing countries is insufficient, with another study showing a contrasting difference between the prevalence of renal calculi in the modern Indian population compared to the same population in previous studies. Study data was restricted in terms of specimen size but it does tend to confirm the general trend in uric acid stone production in the developing world. [3][6][7][8][9]
Pathophysiology
There are three biochemical abnormalities accountable for the formation of uric acid calculi in the renal framework. The most meaningful is the urinary pH, besides other factors, namely hyperuricosuria, and urine volume.
Low urinary pH: The pKa (dissociation constant) of Uric acid is 5.5, at which 50 percent of uric acid is in the form of urate, the soluble form. The remaining 50 percent is in the relatively insoluble uric acid form. The pH of urine can vary considerably. Uric acid is a weak acid, and thus in the presence of an acidic urinary pH (less than 5.5), soluble urate converts into insoluble uric acid. [4]
Low pH of the urine is the primary determinant contributing to stone formation in metabolic syndrome and gouty diathesis. Low urine pH in subjects with metabolic syndrome can be attributed to defective ammoniogenesis.
The two elements that can lead to the acidic pH of urine are: 1) an increase in the net production/excretion of acids and 2) a decrease in the urinary buffering capacity.
The two types of buffers for counteracting excess acid in urine are:
- High capacity ammonium ions (NH4+)
- Low capacity titratable acids
Insulin resistance in metabolic syndrome induces the lipotoxicity of cells in the proximal convoluted tubule (PCT). The following mechanism becomes defective in the absence of insulin:
- Insulin stimulates the metabolism of glutamine in PCT, leading to the formation of two molecules of ammonia and alpha-ketoglutarate.
- Na+/H+ transport in PCT produces H+ in the PCT, which combines with NH3 in the tubular lumen, forming ammonium (NH4+). This ammonium acts as the primary buffer for urinary acid. It is capable of significant variation in response to increasing acid in urine.
- In the absence of NH4+, titratable acids, including phosphates, are responsible for buffering the urine. However, these are not able to respond significantly to urine pH changes, thus leading to an acidic pH and subsequent stone development.
- The underlying mechanism of low urine NH4+ and pH, simultaneously with a drop in NHE3 (sodium hydrogen exchanger-3) activity, due to renal steatosis, was exhibited on the comparison of diabetic fatty rats with lean rats.
Hyperuricosuria can be defined as the daily urinary uric acid excretion of more than 800 mg in men and more than 750 mg in women. It can be the result of numerous congenital and acquired causes, leading to increased uric acid generation or diminished elimination of uric acid. However, it is never singularly accountable for the production of stones. An added biochemical abnormality must also be present.
Low urine volume can lead to supersaturation of lithogenic factors in the urine. The solubility of uric acid is 100 mg/L, at which it remains soluble in urine. However, when the concentration of uric acid reaches 200 mg/L, the maximum stable limit, lithogenic factors start precipitating uric acid crystals which can then lead to stone formation. Thus, the intake of fluid to produce at least 2 - 2.5 liters of urine daily is recommended to avoid urinary supersaturation with lithogenic factors. [4][6][10]
Histopathology
Uric acid stones often look like pebbles with two layers; an outer columnar layer of uric acid crystals enclosing an inner zone of a loose aggregation of uric acid stones, arranged in a concentric fashion.[11]
History and Physical
Patients with nephrolithiasis chiefly present to the emergency department with complaints of flank pain which is radiating towards the lower abdomen. The radiation of pain advances towards the pubic area and then the tip of the genitalia with the stone's passage through the ureter. Pain is intermittent, colicky, and may be quite severe, supplemented by nausea or vomiting. Fever may be present if the stone obstruction is complicated by infection. About 85% of nephrolithiasis patients will have gross or microscopic hematuria, which can help confirm or suggest the diagnosis.
Taking a comprehensive history of a patient diagnosed with nephrolithiasis is very important. The medical history may reveal a history of gout or diabetes mellitus. The patient may be taking medications that enhance uric acid in the urine, such as probenecid or sulfinpyrazone, which interfere with uric acid reabsorption in the kidneys. A dietary history is vital in terms of animal meat protein intake, water input, alcohol consumption, and fructose-containing food intake.
On physical examination, the patient could be in considerable distress due to the pain. Patients may literally writhe in agony and are constantly moving in contrast to those with an acute abdomen who try to remain absolutely still. Nausea and vomiting is often present. Costovertebral tenderness may be present, but often, the abdominal examination is unremarkable. Tophi may be seen in patients with primary gout. [4][10][12][13]
Evaluation
Evaluation of a patient suspected of having nephrolithiasis should invariably commence with a comprehensive history and physical exam.
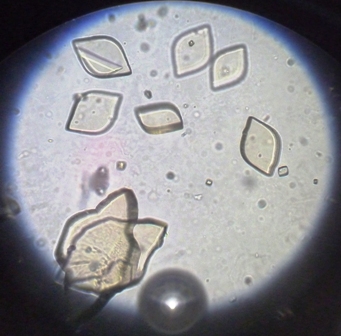
The next recommended step in management is a urinalysis, which includes a urinary dipstick and microscopic examination of the urine for blood and crystals. The dipstick urinalysis will also measure the urinary pH. (An acidic urinary pH favors the presence of uric acid stones.) It can also suggest an underlying infection and should be followed by a microscopic urinalysis, urine culture and sensitivity if the dipstick or microscopic urinalysis shows pus cells in urine. Positive nitrites is also suggestive of an infection. The presence of hematuria is suggestive but not diagnosis of nephrolithiasis. The microscopic urinalysis can also identify urinary crystals which are not apparent on dipstick examinations. The presence of diamond or barrel-shaped crystals of uric acid stones.[14]
Serum chemistry measurements should be done to check the levels of calcium, sodium, potassium, chloride, bicarbonate, and uric acid. (Serum uric acid may need to be ordered separately if it is not part of the automated chemistry panel.) An elevated level of uric acid in serum could suggest the presence of underlying primary gout and increases the likelihood of uric acid urolithiasis.
Stone chemical analysis is suggested whenever possible when a patient presents with the kidney stone. Computerized tomography (CT) scans without contrast are a reliable tool to identify and locate urinary calculi. Non-contrast scans are recommended since intravenous contrast can make stones harder to see. Due to the difference in density, they may also be able to distinguish uric acid calculi from other stones, however, it is usually easier to obtain a plain x-ray of the abdomen. Large calcific stones (>4 mm) should be easily visible on the plain x-ray. If not, then a uric acid stone is more likely. Calculi are classified based on the distinction in the attenuation of rays by separate stones. [15] Chemical composition analysis of the stone can help identify the underlying metabolic disorder and guide further therapy and prophylaxis. [16]
Non enhanced (non-contrast) Helical CT of the abdomen and pelvis is the single most sensitive and specific test for diagnosing urolithiasis. It also can identify radiolucent stones that are not visible on plain abdominal X-rays. A plain abdominal X-ray and a renal ultrasound can be performed if a CT scan is not available. More than 70% of renal calculi are radio-opaque, and thus detectable on X-ray. Ultrasonography has relatively low sensitivity but is indicated in pregnant women and can be useful in patients who come for a follow-up in an outpatient setting. [13] The combination of a plain abdominal X-ray and a renal ultrasound with resistive index determination can be very useful in the diagnosis of urolithiasis when a CT scan is not available or cannot be used. (An obstructing stone will increase the resistive index on the affected side.) Renal ultrasound is also useful in tracking the response of presumed renal uric acid stones to alkalinization dissolution therapy. [16]
Metabolic testing comprises at least one, and sometimes two, 24-hour urine samples. It is indicated and recommended in high-risk patients, recurrent stone formers, and in patients who develop stones for the first time but are highly motivated to minimize future stone production. Patients with intestinal malabsorption disorders, recurrent urinary tract infections, renal tubular acidosis, gout, diabetes mellitus, renal failure, high anesthesia risk, children, and those with a solitary kidney are all high-risk patients and metabolic testing is recommended. The urine is tested for pH, volume, calcium, oxalate, citrate, uric acid, creatinine, sodium, phosphate, magnesium, and qualitative cystine. Sulfates and urea nitrogen in urine can correlate with the intake of animal protein in the diet. [12]
The importance of metabolic testing is that it can assist in determining the stone composition, supervise dietary management, identify specific chemical problems which will help guide therapy. Successful treatment requires significant patient compliance, discipline, and motivation. Evaluation of 24-hour urine testing can be complicated, but excellent published guides are now available for free download on the internet. [17]
Treatment / Management
A significant number of patients with nephrolithiasis present to the emergency department with acute renal colic described as severe pain in the flank region, often associated with nausea/vomiting. In such cases, management of the pain is of utmost priority. Ketorolac can be given as 30 to 60 mg IV or IM loading dose followed by 15 mg every 6 hours. IV acetamenophen and lidocaine have also been used successfully for renal colic pain, but the standard therapy if ketorolac is unsuccessful remains IV opioids. Diclofenac in the dosage of 50 mg orally two or three times in a day can also be used for management. [18]
The first step in the evaluation is to perform a dipstick and microscopic urinalysis and obtain a non-contrast CT scan of the abdomen and pelvis. A plain abdominal x-ray (KUB) is very helpful in tracking the stones over time and in the determination of radiolucency. A radiolucent stone is typically assumed to be made of uric acid unless there is information to the contrary. This can only be confirmed with a chemical composition analysis of the stone.
Urgent intervention with a percutaneous nephrostomy or ureteral stenting is indicated in the following situations: [18]
- Obstruction and infection of the upper urinary tract
- Impending renal failure
- Intractable pain or vomiting
- Obstruction of a solitary kidney
In the most urgent or critical situations, a percutaneous nephrostomy is preferred to minimize manipulation of an infected renal unit.
Management of the uric acid stones is described below:
- Lifestyle intervention: The formation of uric acid stones is often associated with metabolic syndrome, diabetes and insulin resistance in many patients. Therefore, weight loss can be beneficial in the treatment of uric acid stones. Dietary changes in diminishing purine consumption in the form of meat protein can also decrease serum uric acid levels.
- Fluid intake: The American Urological Association recommends an intake of fluids sufficient to produce at least 2.5 liters of urine in a day in all stone formers. Urinary dilution inhibits the supersaturation of lithogenic products and thus prevents stone formation. However, this should be tailored according to the lifestyle, environment, and occupation of individuals. Certain beverages, including tea, coffee, wine, beer, and alcohol, may have chemicals that will increase stone risk, such as oxalate, that can mitigate their benefit of increasing urinary volume and dilution.
- Medical dissolution therapy: Explicit management of uric acid nephrolithiasis can be achieved by medical dissolution therapy. Alkalinization of the urine is the foundation of this treatment with the goal of making the urinary pH around 6.5. Achieving this pH even once a day is adequate for uric acid stone dissolution. Therefore, it is recommended that patients measure their urine pH once a day following the commencement of the treatment. Ultrasound can be used to track the progress of therapy. Continuing treatment with alkalinizing agents is the recommended maintenance therapy for most uric acid stone formers.
Bicarbonate salts of sodium and potassium are generally used to alkalinize the urine. Potassium citrate therapy is the first-line medication available for uric acid stones. It is given in the dosage of 20 to 40 mEq once or twice in a day. However, it should be avoided in patients with reduced glomerular filtration and patients taking angiotensin-converting enzyme inhibitors and angiotensin receptor blockers. Sodium bicarbonate, being economical, has been used extensively for uric acid stones. However, it carries a high sodium load which can worsen hypertension, congestive heart failure, and cirrhosis due to fluid retention. Acetazolamide can prove useful in such cases as it is an inhibitor of bicarbonate excretion and leads to diuresis and alkalinization of urine, but it reduces urinary citrate excretion.
Theobromine found in cocoa products has been found to promote the alkalinization of urine. Theobromine has been witnessed to repress the formation of uric acid stones by hindering the nucleation method plus rebuilding the morphology of uric acid stones. Theobromine is thought to substitute the uric acid molecules in crystals, modifying them into potent molecules and minimizing their growth. Theobromine also inhibits the recurrence of stone formation post extracorporeal shock wave lithotripsy.
Allopurinol is not routinely recommended for patients with uric acid calculi. It is only advised if the urine's alkalinization is not adequate or if there is hyperuricosuria or hyperuricemia.
The patient should have follow-up imaging studies to assess the location of the stone and detect any complications. The patient is also directed to strain the urine and retrieve the stone for chemical composition analysis. Expectant management can usually be done for 4-6 weeks. If the stone passes, additional follow up is done by 24-hour urine metabolic testing to begin specific kidney stone prophylactic treatment. However, if the stone is still present and has not moved, surgical intervention will be needed. Targeting the radiolucent stone may be difficult with only fluoroscopic guidance in shock wave lithotripsy, although this can be achieved by using retrograde pyelography. Ureteroscopy with laser lithotripsy is an efficient technique for surgical management of most uric acid stones requiring surgical intervention. [7][10][12][13][16][18][19][20]
Differential Diagnosis
The following conditions should be kept in mind when a patient presents to the emergency with abdominal pain:
- Pyelonephritis
- Ruptured ectopic pregnancy
- Appendicitis
- Aortic aneurysm rupture
- Prostatitis
- Differentials of radiolucent stones:
- Xanthine stones - These stones are usually seen in people who are on allopurinol and are hyperuricemic.
- Matrix stones
- Ammonium urate (associated with laxative abuse)
- Medication stones (usually of one of several medications that can form urinary stones such as crixivan)
- 2,8-dihydroxy adenine stone formation occurs in patients with a deficiency of adenine phosphoribosyltransferase.[21]
Prognosis
A follow-up of a patient with renal calculi should include imaging studies to evaluate for stone progression and activity. Though 80% to 90% of stones pass spontaneously if 4 mm in size or less, in the remaining cases immobile calculi can lead to obstruction, infection, pyonephroisis, caliceal rupture, urinomas, loss of renal parenchyma and ureteral strictures. Uric acid stones are well managed by alkalinization therapy, but surgery can be performed in the case of calculi >10 mm. The underlying etiology also determines the prognosis of uric acid calculi. [13]
Complications
- Hydronephrosis
- Obstructive pyelonephritis
- Recurrent urinary tract infections
- Ureteral perforation
- Caliceal rupture with urinoma formation
- Ureteral strictures
- End-stage renal disease
- Chronic kidney disease
- Stone recurrences
Deterrence and Patient Education
Patients with uric acid stones should be educated about incorporating a healthy lifestyle. Modifications in the diet, weight, and physical activity are necessary as uric acid stone formation has been connected to insulin resistance and obesity. Diet should be revised to minimize animal protein intake while also avoiding food with high fructose and salt content. Patients should drink sufficient fluids to limit urinary supersaturation. Patients should also be educated to recognize the signs of complications, including fever and anuria, and they should immediately consult their physician. High-risk cases and all kidney stone patients strongly motivated to optimize preventive measures, should be offered 24-hour urine testing to identify their treatable risk factors for recurrent stone disease. [18]
Enhancing Healthcare Team Outcomes
The management and prognosis of a patient with uric acid nephrolithiasis improve with efficient communication amongst the interprofessional team of healthcare providers, which includes an emergency department physician, primary care physician, urologist, and nephrologist. The management of a case of uric acid nephrolithiasis starts mostly in the emergency department with the treatment of colicky pain. However, an urgent referral to the urologist may be needed if a need for immediate intervention is present. The primary care physician and the nurse practitioner provide an indispensable role in remodeling the lifestyle of the patient. Uric acid stones are associated with cardiometabolic diseases; thus, they could be seen as warning signs of these diseases.
It is imperative to motivate the patient between the occasional episodes of pain to get the metabolic testing done. The physician should use the ROKS nomogram to evaluate the recurrence of stone and order 24-hour urine testing as required. Only about 7.4% of patients undergo successful 24-hour urinary testing due to inconvenience related to the test and its interference with daily activity.
The American Urological Association has provided guidelines for the management of uric acid nephrolithiasis, which is based on a systematic review and has been extensively peer-reviewed. Interprofessional communication between different practitioners is very crucial to adhere to these guidelines and improve disease outcomes. [12][20]