Continuing Education Activity
Eyelid lacerations are managed differently depending on the depth, width, and location of the injury. Surgical management will be broken down into these categories: laceration without eyelid margin involvement, laceration with eyelid margin involvement, and laceration with nasolacrimal system involvement. This activity describes the types of eyelid lacerations, their repair, and potential complications.
Objectives:
Describe the anatomy of the eyelid.
Review the indications for an eyelid laceration repair.
Summarize the technique for repairing an eyelid laceration.
Explain the importance of improving care coordination among the interprofessional team to enhance care delivery for patients undergoing repair of an eyelid laceration.
Introduction
Eyelid lacerations are managed differently depending on the depth, width, and location of the injury. Surgical management will be broken down into these categories: laceration without eyelid margin involvement, laceration with eyelid margin involvement, and laceration with nasolacrimal system involvement.
Anatomy and Physiology
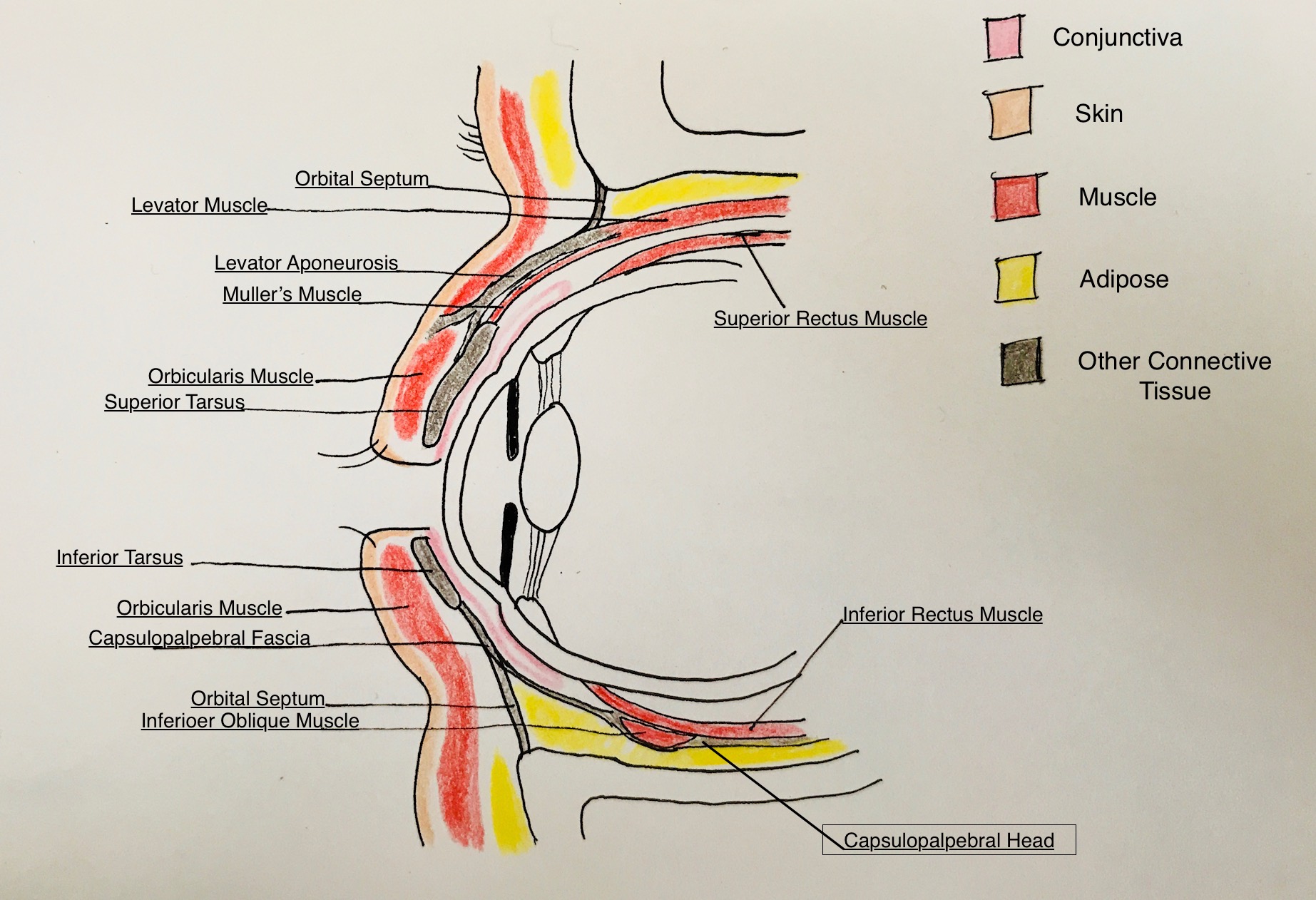
It is important to be proficient in eyelid anatomy when addressing an eyelid laceration (see Image. Eyelid Anatomy). The eyelid has multiple layers that serve different functions, as described below. Please see the eyelid anatomy illustration for correlation.
Skin/Subcutaneous Tissue
The eyelid skin is unique because it has no subcutaneous fat and is thus the thinnest layer of the body's skin. The skin overlying the tarsus tends to be firmly attached to the underlying tissue; whereas, the skin above the tarsal plate over the orbital septum is loosely attached to underlying tissue giving rise to a potential space for fluid to collect in the setting of trauma/edema. Because eyelid skin is very thin, a smaller diameter suture is required, and smaller bites are taken when approximating lacerations that only involve eyelid skin.
Protractors
Directly under the upper and lower eyelid skin is the orbicularis oculi muscle. This is the main protractor muscle of the eyelid (eyelid closure). The orbicularis oculi muscle is a large, thin, circular muscle divided into pretarsal, pre-septal, and orbital parts. The pretarsal and pre-septal parts are responsible for involuntary eyelid closure (blinking). The orbital portion is primarily responsible for voluntary/forced eyelid closure.
Orbital Septum
A thin, fibrous connective tissue layer separates anterior eyelid structures from intra-orbital structures. The upper orbital septum connects the periosteum of the superior orbital rim to the levator aponeurosis above the superior tarsal border (though this has racial variance). The lower orbital septum connects the periosteum of the inferior orbital rim to the capsulopalpebral fascia just below the inferior tarsal border.
Orbital Fat
This is located immediately posterior to the orbital septum and anterior to the levator aponeurosis in the upper lid and capsulopalpebral fascia of the lower lid. In the upper lid, there are discrete nasal and central fat pads. In the lower eyelid, there are three fat pads: nasal, central, and temporal. The pads are surrounded by thin fibrous capsules. The central orbital fat pad is an important landmark in lid laceration repair due to its locations directly posterior to the orbital septum and anterior to the levator aponeurosis.
Retractors
Upper Eyelid
The levator muscle originates in the apex of the orbit, travels forward over the eyeball, and splits into two different structures: the levator aponeurosis anteriorly and the superior tarsal muscle (Muller's muscle) posteriorly. The split occurs superiorly at the Whitnall ligament and inferiorly at the Lockwood ligament.
The levator aponeurosis continues inferiorly and splits into an anterior and posterior portion near the upper tarsal border. The anterior portion of the levator aponeurosis inserts into the pretarsal orbicularis and skin to form the upper eyelid crease. The posterior portion of the aponeurosis inserts into the upper anterior surface of the tarsal plate.
Muller's muscle extends from the undersurface of the levator aponeurosis at the level of the Whitnall ligament and inserts along the upper eyelid superior tarsal margin. It is a sympathetically innervated retractor muscle of the upper eyelid.
Lower Eyelid
The capsulopalpebral fascia is analogous to the levator aponeurosis in the upper eyelid. Its fibers originate from attachments to the inferior rectus muscle. It extends forward, envelops the inferior oblique muscle, forms the Lockwood ligament, and continues anteriorly, attaching to the orbital septum and inferior conjunctival fornix before finally inserting at the inferior tarsal border.
The inferior tarsal muscle is analogous to the Muller's muscle in the upper eyelid. This muscle is poorly developed and runs posterior to the capsulopalpebral fascia of the lower eyelid.
Tarsus
The tarsal plates serve as the main structural components of the eyelids. They are made of dense connective tissue and contain the Meibomian glands and eyelash follicles. The tarsal plate of the upper eyelid is 10 mm to 12 mm vertically in the center of the eyelid, and the tarsal plate of the lower eyelid is up to 4 mm vertically in the central eyelid. Both tarsal plates have rigid attachments to the periosteum via the medial and lateral canthal tendons.
Conjunctiva
This non-keratinizing squamous epithelium lines the inner surface of the eyelids and continues to cover the anterior surface of the eyeball, where it terminates at the edge of the cornea. It contains mucin-secreting goblet cells and accessory lacrimal glands that assist in keeping ocular tissues lubricated.
In the nasolacrimal system (not represented in the illustration), both the upper eyelid and the lower eyelid have small openings on the surface of the eyelid margin near the medial canthus. These are called puncta. The puncta lead to a drainage tube called the canaliculus which, eventually, drains into the lacrimal sac and out of the nose via the nasolacrimal duct. Within the eyelid, the canaliculus travels 2 mm inferiorly from the punctum, then turns 90 degrees medially and travels 8 mm to 10 mm before reaching the common canaliculus (where both upper and lower canaliculi meet). The common canaliculus drains tears into the lacrimal sac and down inferiorly into the nasolacrimal duct. The fluid can then exit underneath the inferior turbinate in the nose.[1][2][3][4]
Indications
Any injury that disrupts the structure and/or function of the eyelids can cause the condition. Generally, an eyelid skin laceration greater or equal to 2 linear millimeters requires repair.
Contraindications
There are no absolute contraindications to eyelid laceration repair; however, in patients with concurrent globe rupture, the globe should be evaluated and repaired before any lid procedure. Lacerations secondary to heavy contamination or human/animal bites may need minimal necrotic tissue debridement, but a primary repair is often still performed. Nonetheless, contaminated wounds may be left open for delayed repair.
Using local with epinephrine is relatively contraindicated in patients with Raynaud phenomenon, sickle cell disease, arteritis, or severe microvascular disease, but necrosis of the eyelid following lidocaine with epinephrine administration is very rare.
Equipment
- Castroviejo needle driver
- Castroviejo 0.5 mm forceps
- Suture (6-0 silk, 6-0 plain gut, 6-0 polyglactin)
- Cautery
- Stents (if needed)
- Standard prep materials for the sterile procedure
Personnel
Non-marginal and non-canalicular system-involving lacerations involving eyelid skin can be repaired by the emergency room clinician, general plastic surgery, or primary care providers. An ophthalmologist or oculofacial plastic surgeon should perform complex lacerations involving the eyelid margin, canalicular system, or canthal tendons.
Preparation
Consider tetanus prophylaxis. Obtain appropriate radiologic studies. Determine the appropriate setting for repair, such as operating room (OR) versus bedside.
Indications for OR repair include nasolacrimal system involvement, levator aponeurosis/superior rectus involvement, violation of orbital septum/visible orbital fat, canthal tendon avulsion, extensive tissue loss (more than one-third of the eyelid).
- Position the patient in the supine position.
- Instill topical anesthetic in each eye. Place a protective scleral shell over the affected eye. Irrigate the surrounding skin and clean it with a full-strength povidone-iodine solution. Ensure any foreign body or particulate matter is evacuated from the wound. Isolate the area with sterile drapes.
- If the canalicular system is involved, pack the nasal cavity with oxymetazoline and 4% lidocaine-soaked neuro sponges.
- Administer local subcutaneous anesthetic (2% lidocaine with 1 in 100,000 epinephrine) using the minimal amount necessary for adequate anesthesia.
Technique or Treatment
Simple, Superficial Eyelid Laceration Repair
Reapproximate skin edges with simple interrupted sutures using 6-0 silk or 6-0 plain gut suture. Be sure to evert the skin edges. Take small bites (approximately 1 mm from the skin edge) and space sutures 2 mm to 3 mm apart. Avoid tightly tying sutures to the skin. Tight sutures can strangulate delicate tissue. The silk suture will need to be removed. The plain gut suture is absorbable and is preferred if the patient is not reliable to follow-up for suture removal.
Eyelid Margin Involving Laceration
Many techniques are commonly employed to approximate the edges of an eyelid margin laceration.
- Using 6-0 Silk suture, re-approximate the edges of the eyelid margin by placing one simple interrupted suture from gray line to gray line. Do not tie the suture. See Image 2a.
- Then, place partial-thickness simple interrupted sutures using 6-0 Vicryl to approximate the edges of the tarsal plate. Tie these sutures and cut the ends short. This is important for the structural integrity of the eyelid.
- Place an additional marginal 6-0 silk suture parallel to the first but closer to the lash line.
- Suture skin as described above.
Eyelid Laceration with Canalicular Involvement
Dilate both upper and lower puncta. If there is an un-involved punctum, probe it to the sac and irrigate to ensure there are no underlying blockages. Then identify the medial and lateral ends of the lacerated canaliculus. A miniaturized stent can be used if only one canaliculus is involved. If both are involved, silicone tubing or a Crawford stent can be used. See below for stenting techniques for miniature and Crawford Stent. Suture skin as described above in simple laceration repair.
Miniature stent: Advance a stent through the punctum of the lacerated canaliculus and out the distal end. Then insert a stent into the canaliculus opening of the lacerated lateral edge. Ensure the stent is seated in the punctum. Place several 6-0 polyglactin sutures using a curved needle to anastomose the cut edges of the canaliculus and re-approximate the surrounding tissue. Leave these untied. Then place addition interrupted buried 5-0 polyglactin sutures to reinforce the medial canthal tendon. After all deep sutures are placed, tie and trim all sutures.
Crawford Stent: Place the first end of the stent through the punctum of the lacerated canaliculus and out the distal end. Then pass the same end through the previously identified proximal end and then advance through the lacrimal and nasal lacrimal duct. Retrieve the end of the stent from the nasal cavity. Pass the other end of the stent similarly through the intact canaliculus. Tie and trim ends in the nose just before skin closure.[5][6][7][2][8][9]
Complications
Complications of eyelid lacerations that do not involve the canalicular system include missed injury, infection, eyelid notching, irregular eyelid contour, lagophthalmos, exposure keratopathy, septal perforation, prolapse of orbital fat, corneal injury, shortening of eyelid fornices, wound dehiscence, entropion, trichiasis, and hemorrhage.
Additional complications include lacerations involving the canalicular system, such as epiphora, stent migration, and epistaxis.[10]
Clinical Significance
Maintaining the proper position and structure of the eyelid is extremely important for adequate tear film, tear drainage, protection of ocular surfaces, and cosmesis. Eyelid lacerations disrupt the normal anatomy of the eyelid and require careful repair to prevent ocular surface decompensation and unnatural cosmesis.
Enhancing Healthcare Team Outcomes
Patients with eyelid lacerations often present to the emergency department or the urgent clinic. The emergency department physician may manage a simple eyelid laceration, but all other lacerations should be referred to the ophthalmologist or plastic surgeon. Prior to any repair, the ophthalmic nurse should assess the patient's visual acuity. Complex eyelid lacerations are often associated with other eye injuries, which require a full evaluation prior to repair. The outlook for simple eyelid lacerations is excellent. All interprofessional team members, including clinicians, specialists, mid-level providers, pharmacists, and nursing staff, must work as a cohesive unit to optimize patient outcomes in these procedures. [Level 5]