Introduction
The prostate is a "walnut-shaped gland, a part of the male reproductive system that produces and secretes thin alkaline fluid in the ejaculate. It contains glandular and stromal elements that are subject to enlargement and developing adenocarcinoma in an elderly patient. Infection is common in relatively younger patients. Imaging plays a vital role in the diagnosis of different prostatic pathology, including early detection of carcinoma. Imaging also helps obtain tissue samples, drain abscess and post-procedure collections, and stage and follow malignancy.
Anatomy
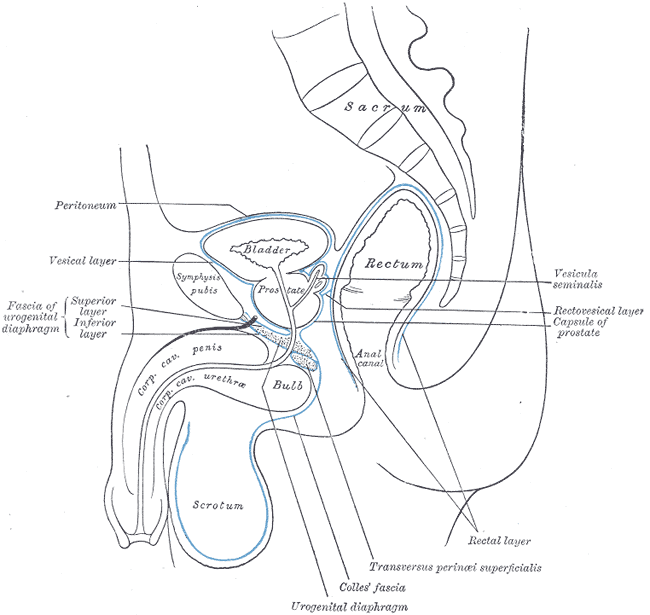
The prostate is located in the pelvic cavity inferior to the urinary bladder surrounding the prostatic urethra. The gland comprises an apex resting on the urogenital diaphragm, a base attached to the bladder neck, and inferolateral surfaces resting on the levator ani facia above the urogenital diaphragm. See Image. Median Sagittal Section of Male Pelvis Anatomy.
Anatomically, it is divided into two lateral (right and left) and one median lobe. Histologically, it has a central zone (CZ) comprising 25% of the prostatic mass that forms the base; a peripheral zone (PZ) surrounding the central part constituting 25% of the prostatic mass; and a transition zone(TZ) that surrounds the anterolateral portion of the urethra in a horseshoe-like fashion. It is essential to know these histological zones because 70% of the adenocarcinomas arise from the peripheral zone while 20% from the transition zone. Only 10% of adenocarcinomas arise from the central zone. Prostatitis more often occurs in the central zone. Benign prostatic hyperplasia typically expands the transitional zone creating adenoma.
Plain Films
Plain radiographs have limited prostate evaluation utility but are rarely used as a skeletal survey to assess or follow metastases.
Other imaging modalities like bone scan are used for assessing bone metastases, and CT of the chest, abdomen, and pelvis are used to stage prostate cancer. MRI of the prostate is sensitive and specific for assessing prostate malignancy and local extension. CT/MRI is also used to place radiation seeds before radiotherapy.
Computed Tomography
Detailed prostate anatomy is not well defined on the CT scan, as its pathology. It may show a hyperdense central zone with density adjusted around 40 to 60 Hounsfield Unit (HU), and the peripheral zone may appear hypodense between 10-5 HU density.
BPH
CT scan is not typically done for diagnosis, but BPH is identified when the prostate extends above the pubic symphysis on axial imaging. BPH can also be diagnosed on a CT scan with a volume greater than 30 ml (measured with the help of coronal reformate images).
Prostate Inflammation
In prostatitis, the gland appears diffusely hypodense with symmetric or asymmetric enlargement. Prostatic abscesses are well-defined hypoattenuating (approximately fluid density, around -19 to 13 Hounsfield unit) areas with peripheral rim enhancement. Progression of the disease can be monitored with a CT scan or alternative to the sonography.[1]
Prostate CA
Prostatic malignancy appears as contrast-enhancing areas, particularly in the venous phase. These areas can be focal or diffuse and are found within the peripheral zone. CT scan has a role in carcinoma imaging to assess local and distant spread.[2]
Magnetic Resonance
Magnetic resonance imaging (MRI) is an excellent modality for prostate imaging due to its better contrast resolution. MRI can differentiate anatomical zones and their abnormalities. Prostate MRI is performed with a pelvic coil and is sensitive in detecting malignancy and assessing its local extension. The use of an endorectal coil provides more information and better resolution (see Image. MRI of Normal Prostate Using Endorectal Coil). With recent advances like multiparametric MRI (mp-MRI), functional MRI, and an MRI-guided biopsy, MRI is increasingly useful in detecting low-grade or low volume prostate carcinoma. Necessary MRI sequences include T2 weighted, diffusion-weighted imaging (DWI) along with an apparent diffusion coefficient (ADC) and dynamic intravenous contrast-enhanced (DCE) imaging. DWI analyzes the diffusion of water molecules at the cellular level. ADC is a qualitative measure of average water diffusion per voxel. DWI is particularly important in the diagnosis of prostate carcinoma and prostatitis, including abscess.[3]
Normal Anatomy
The peripheral zone is homogeneously hyperintense on T2 weighted imaging (T2WI) with the hypointense capsule. The transition zone shows heterogeneity while seminal vesicles appear uniformly hyperintense on T2WI.
BPH
MRI delineates zonal anatomy, its elements, and gland volume as well as zonal volume. BPH appears as heterogenous TZ on T2WI. Due to glandular or stromal tissue enlargement, enlarged nodules in BPH show increased or decreased signals on T2WI. Glandular enlargement appears as bright signals on T2WI, while fibromuscular and stromal elements are dark on T2WI. Estimation of stromal and glandular ratio helps to choose appropriate medical therapy.[4] Stromal enlargement may mimic transitional zone cancer due to low intensity on T2WI, diffusion restriction, and contrast enhancement, similar to prostatic carcinoma. Stromal hyperplasia can be differentiated by having a more well defined and encapsulated appearance.[5]
On MRI, BPH can be divided into seven types. Type 0= no/little zonal enlargement. Type 2= retrourethral. Type 3= retrourethral+ bilateral TZ. Type 4= pedunculated (multiple or solitary). Type 5= pedunculated + bilateral TZ +/- retrourethral. Type 6= subtrigonal or ectopic enlargement. Type 7= other combinations. Besides diagnosing BPH, MRI plays an important role in identifying carcinoma when a patient with BPH has increased PSA and suspicious or at high risk for developing prostate cancer.[4]
Prostate Infection
Bacterial prostatitis is acute or chronic and is more common in the peripheral zone. Acute prostatitis appears T2 hyperintense with increased contrast enhancement. Chronic prostatitis is usually hypointense on T2 and shows poor contrast enhancement. Chronic prostatitis demonstrates increased diffuse restriction due to inflammatory cell infiltrate. These findings mimic prostatic carcinoma. However, the degree of diffusion restriction is lower than carcinoma. Non-necrotic granulomatous prostatitis also appears hypointense on T2 with diffusion restriction, but on the contrary to chronic prostatitis, there is no enhancement on postcontrast imaging. The necrotic area of granulomatous prostatitis shows an increased signal on T2WI. In patients with extra-prostatic extension of the granulomas, it's challenging to differentiate them from carcinoma.[5][6]
Prostatitis may progress into abscesses, which is hyperintense on T2, hypointense on T1, and shows peripheral contrast enhancement. The abscesses show diffusion restriction and low ADC value.[7]
Prostate Malignancy
Prostate carcinoma is related to high morbidity and mortality worldwide. MRI, specially mp-MRI, is useful for cancer detection and helps to avoid unnecessary biopsy. Pre-biopsy MRI and MRI guided biopsy is more superior to the TRUS guided biopsy.[8] Pre-biopsy MRI helps avoid over staging errors that may occur due to biopsy artifact.[9] MRI also detects anterior, lateral, and apex tumors, which may be missed by biopsy. The malignant lesions are typically in the peripheral zone with T2WI hypointensity, focal enhancement, and low diffusivity. Ill-defined and T2 hypointense lesions in PZ is highly suspicious for carcinoma. Though malignancy is less common in the transition zone, non circumscribed, spiculated, relatively T2 hypointense lesions are suspicious.
MRI is also used to assess metastases that are not visualized on the bone scan or CT. It's also used to evaluate pathological fractures and associated complications.
PI-RADS- Prostate Imaging Reporting and Data System is a standardized classification based on mp-MRI findings updated in 2015, known as PI-RADS version 2 = PI-RADS™ v2. According to it, the presence of clinically significant carcinoma is categorized into the following:
- PI-RADS 1- Highly unlikely-Normal T2WI and DW/ADC.
- PI-RADS 2 – Unlikely-Circumscribed heterogeneity on T2WI and hypointensity PZ on DW/ADC (see Image. MRI Prostate, PIRADS-3).
- PI-RADS 3 – Equivocal- Heterogenous lesion with obscured margin on T2WI; hyperintense on DW & hypointense on ADC.
- PI-RADS 4 –Likely- Non circumscribed </= 1.5 cm lesion, moderately homogenously hypointense on T2WI; hyperintensity on DW & hypointense on ADC (see Image. MRI Prostate, PIRADS-2).
- PI-RADS 5 – Highly likely- similar to PI-RADS 4 but lesion > 1.5 cm or extra-prostatic extension.
Ultrasonography
Ultrasound is widely available for prostate evaluation but also for performing guided prostatic biopsy. Transabdominal (TAUS) or transrectal (TRUS) sonography can be used to evaluate the prostate, and transrectal is preferred for biopsy. See Image. Transrectal Ultrasound Guided Biopsy of the Prostate. The prostate is examined with TAUS by a transducer placing just above the pubic symphysis with a fluid-filled urinary bladder serving as an acoustic window. The average normal measurements are 3.75 to 4.00 × 2.5 to 3.00 × 3.1 to 3.8 cm (width x height x length) with a volume of 20 to 25 cm. The prostate volume is calculated using the formula for measuring any ellipsoidal structure is 0.5236 × height (H) × width (W) × length (L).[10]
TAUS is limited in obese patients, and in those, bladder filling is not possible to correctly evaluate prostate volume. TRUS is performed in such cases. TRUS is also necessary for suspected prostatic pathology during the clinical exam, increased prostate-specific antigen (PSA) in the blood serum, prostatic inflammation/abscess, and follow up of prostatic cancer, as TRUS allows detailed evaluation of the prostate.
For TRUS, an endorectal transducer having a frequency of 8 to 10 MHz is delicately inserted into the rectum. Prostate volume is measured similarly to TRAS by obtaining width, height, and length. The gland is evaluated for its shape, symmetry, echogenicity, and integrity of the prostatic capsule. Periprostatic structures, e.g., seminal vesicles, neurovascular bundles, and blood vessels, are assessed for any abnormality, especially in suspected prostate carcinoma.[11]
Elastography is a vital aid performed during TRUS to evaluate the firmness of the prostate tissue. The areas of increased firmness are often identified on elastography, which does not show any abnormal echogenicity on grayscale imaging.
Benign Prostatic Hyperplasia
TAS OR TRUS assesses the prostate volume to determine the course of management, i.e., prostatic volume more than 80 cm3 qualifies for open surgery-adenomectomy; otherwise, transurethral resection is the choice for management. European Association of Urology (EAU) suggests measuring prostatic volume via TRUS and residual urinary bladder post-void urine volume through TAUS. Ultrasound examination should be supplemented by visualization of the upper urinary tract to assess the degree of urinary tract dilatation.
Prostate Inflammation
Prostatitis is usually a clinical diagnosis. Sonography in prostatitis frequently demonstrates an enlarged and/or deformed gland with inhomogenous echotexture. Acute prostatitis may result in a parenchymal abscess, which appears as a hypoechoic or fluid consistency lesion within the prostate parenchyma. Ultrasound is performed not only for diagnosis but also for planning to evacuate it under ultrasound guidance. Ultrasound is useful in intraprostatic antibiotic injections in chronic prostatitis when pain is exacerbating.[12]
Prostatic Neoplasm
Prostatic malignancy is difficult to diagnose in the USG as the tumor is often isoechoic to the surrounding normal gland. It could be hypoechoic. The US with color Doppler or power Doppler can identify angiogenesis, showing dilated and tortuous vessels, but it cannot detect small tumor foci. The diagnostic value of ultrasound is around 30% to 40%.[11] Therefore, it's mostly used as a guidance for prostatic biopsy. It is proven to improve cancer detection, especially in men who have a positive PSA and PSA ratio.[13] The US is often helpful in identifying local tumor spread and thus staging cancer.
Some advances, like elastography, identify consistency difference and help in tumor diagnosis and guided biopsy. On elastography, neoplasm consistency appears firmer than the surrounding normal tissue. 3D TRUS allows computer processing of sectional images of the prostate and adds more detailed information about the morphology, surrounding structures, etc.[11] The contrast-enhanced US has a high sensitivity to differentiate neoplasm from normal prostate tissue and more useful for US-guided biopsies.[14]
Nuclear Medicine
Nuclear medicine plays a role in the diagnosis, staging/re-staging, and therapy of prostate carcinoma. Skeletal metastases can be identified with a bone scan. Positron emission tomography (PET) is an examination that assesses malignant activity and its spread in the body. In particular, choline derivative radiotracer, 18F-fluorocholine (F-FCH), is the currently used tracer for diagnosing prostate carcinoma. PET, when combined with CT (PET/CT) and MRI (PET/MRI), adds metabolic/functional data derived from PET to CT or MRI findings.[15][16]
Prostate-specific membrane antigen (PSMA) is expressed on the cell surface of carcinoma, nodal metastasis, and metastases to the bones. Ga-labeled PSMA inhibitor is a widely used PET tracer, is now becoming popular, not only for diagnosis but also for therapy.[16]
Angiography
Angiography can be utilized for prostatic artery embolization (PAE) in patients with BPH and bleeding. It is an interventional technique in managing patients with lower urinary tract symptoms (LUTS) secondary to benign prostatic hyperplasia (BPH). PAE improves LUTS.
Clinical Significance
Prostate imaging plays a vital role in identifying various pathology, including infection, enlargement, and carcinoma. It is crucial in staging the carcinoma. PI-RADS is a standardized classification based on MRI findings, which helps in further management. US or MRI guided procedures are also widely used for diagnosis as well as therapy.