Continuing Education Activity
Blockade of the suprascapular nerve is an effective modality to treat chronic, acute, and post-surgical shoulder pain. An anterior and a posterior approach to the suprascapular nerve block have been described. This review will describe the relevant anatomy, indications, and ultrasound-guided techniques for both approaches to blocking the suprascapular nerve. This activity highlights the role of the interprofessional team involved in performing a suprascapular nerve block.
Objectives:
- Identify the anatomic structures involved in both techniques to block the suprascapular nerve.
- Describe the technique for performing an anterior or posterior suprascapular nerve block.
- Summarize the potential indications for a suprascapular nerve block.
- Explain the alternatives to suprascapular nerve block.
Introduction
Blockade of the suprascapular nerve is an effective method for providing anesthesia and analgesia for the shoulder. The suprascapular nerve contributes to the sensory innervation of the acromioclavicular and glenohumeral joints, as well as motor innervation of the supraspinatus and infraspinatus muscles. The suprascapular nerve can be specifically targeted to provide shoulder analgesia while potentially sparing blockade of the phrenic nerve.[1][2] This procedure is usually performed as an alternative to the interscalene brachial plexus block, which routinely causes hemi-diaphragmatic paralysis via phrenic nerve blockade.[3]
There are two well-described techniques for blocking the suprascapular nerve. The first is the landmark-based posterior approach, first reported in 1941 by Wertheim and Rovenstein to treat severe chronic shoulder pain. Subsequently, nerve stimulation and ultrasound guidance have been used to identify and block the suprascapular nerve more reliably. However, the posterior approach remains challenging because of the small diameter of the nerve and its anatomic location within the suprascapular fossa, beneath the trapezius and supraspinatus muscles.[4]
In 2012, Andreas Siegenthaler and colleagues described a novel, ultrasound-guided anterior approach to the suprascapular nerve block.[5] This review will address the indications, sonoanatomy, technique, and potential complications for posterior and anterior approaches to blocking the suprascapular nerve.
Anatomy and Physiology
The suprascapular nerve comprises motor and sensory fibers originating from the 5th and 6th cervical spinal nerves; occasionally, fibers from the 4th cervical spinal nerves also contribute.[6][7] The fibers that make up the suprascapular nerve are initially contained within the upper trunk of the brachial plexus, though the nerve branches from the upper trunk within the neck and courses laterally parallel to the inferior belly of the omohyoid muscle and toward the superior border of the scapula. The nerve enters the suprascapular notch and runs through the suprascapular canal under the supraspinatus fascia. The nerve emerges from the suprascapular canal after exiting the spinoglenoid notch and into the infraspinatus fossa.
Before entering the suprascapular canal, branches in the supraspinous fossa provide motor innervation to the supraspinatus muscle. Afterward, emerging from the spinoglenoid notch, branches in the infraspinous fossa to innervate the infraspinatus muscle. In this way, the suprascapular nerve contributes to the abduction of the arm via the supraspinatus muscle and external rotation of the shoulder via the infraspinatus muscle. Sensory branches innervate both the acromioclavicular and glenohumeral joints, but other nerves also contribute to the sensory innervation of the shoulder joints. The glenohumeral joints also receive sensory innervation from the axillary nerve, the lateral pectoral nerve, and the nerve to the subscapularis. The acromioclavicular joint also receives sensory innervation from the lateral pectoral nerve.[8]
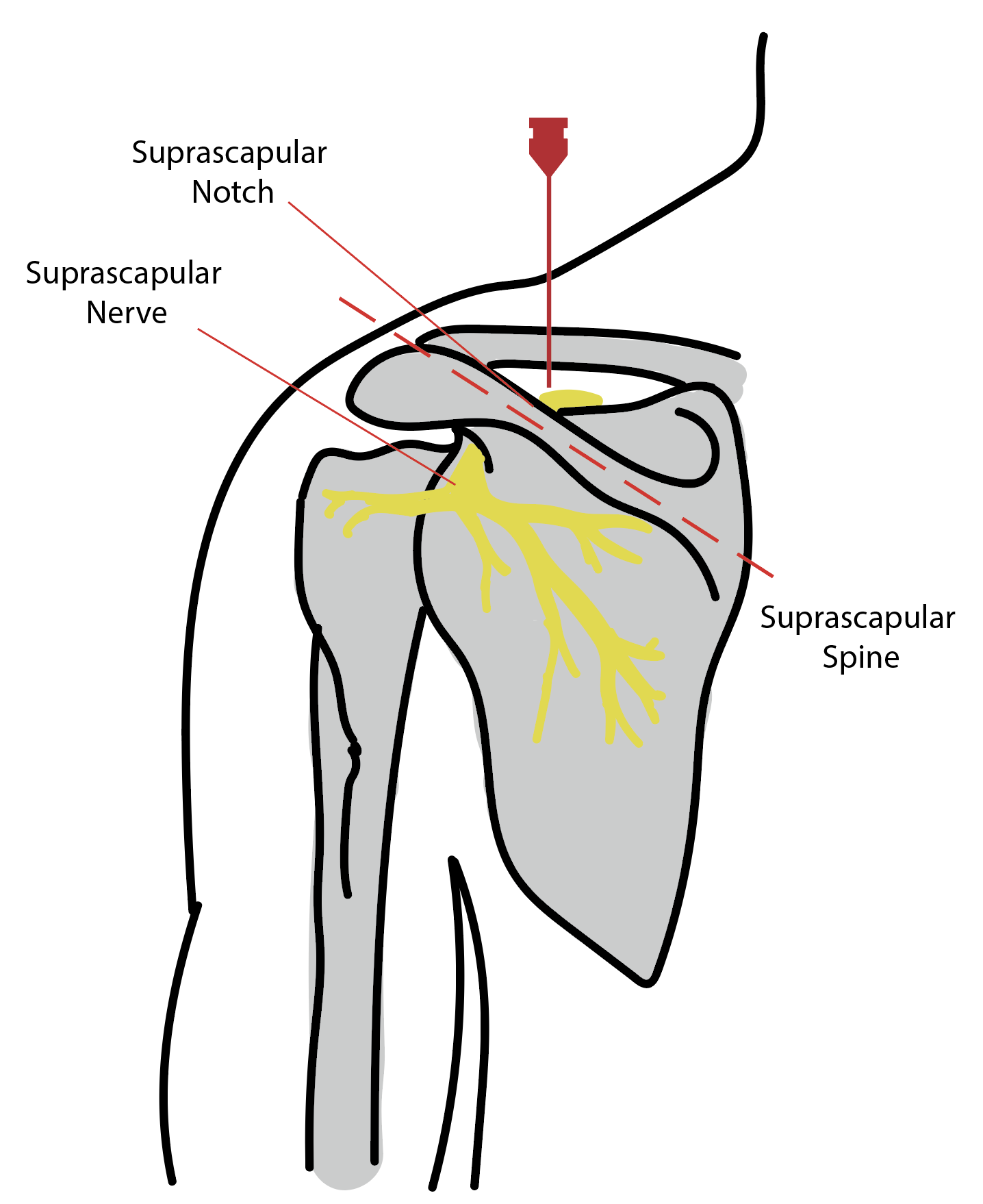
Positioning a high-frequency ultrasound probe anterior to the scapular spine in the coronal plane will produce an image slicing through skin, subcutaneous tissue, trapezius muscle, and supraspinatus muscle before it is reflected by the floor of the scapular spine. Tilting the ultrasound probe in the cephalo-caudad direction should reveal the suprascapular nerve and artery within a slight depression of the scapula (see Figure 1)
The anterior approach identifies the suprascapular nerve just lateral to the supraclavicular brachial plexus below the omohyoid muscle. See Figure 2 for the relevant sonoanatomy.
Indications
A suprascapular nerve block can be utilized to treat chronic, acute, and perioperative shoulder pain. The first description of this block in 1941 was performed to treat a patient with “intractable” shoulder pain. Patients with chronic pain conditions including but not limited to inflammatory arthritis, rheumatoid arthritis, adhesive capsulitis, rotator cuff tendonitis, bursitis, degenerative disease, post-surgical and post-stroke chronic shoulder pain may benefit from a suprascapular nerve block.[9][10][11]
A suprascapular nerve block may be even more beneficial in post-trauma or surgical patients due to the particularly intense and disabling quality of acute shoulder pain.
In the perioperative setting, a suprascapular nerve block is specifically indicated to control shoulder pain in patients with significant pulmonary comorbidities that make an interscalene brachial plexus block contraindicated due to the motor blockade of the phrenic nerve.[12]
Contraindications
As the suprascapular nerve block is an optional procedure to treat pain, patient refusal is an absolute contraindication. Inability to cooperate during the procedure is a relative contraindication, as most peripheral nerve blocks are done in awake patients to receive patient feedback that may alter needle positioning. However, performing otherwise indicated peripheral nerve blocks under general anesthesia is considered safe, specifically when using ultrasound guidance.[13]
Patients with proven allergies to all local anesthetics will not be able to receive peripheral nerve blocks, although this is exceedingly rare.
Equipment
- A diagnostic ultrasound machine is used to perform ultrasound-guided peripheral nerve blocks. Ideally, the device should have a high frequency (5 to 13 MHz) linear probe for superficial structures and the option to use a low frequency (2 to 5 MHz) curved array probe for deeper structures.
- The echogenic short bevel block needle is commonly used for single-injection nerve blocks. Still, a 17-gauge Touhy needle may be used to facilitate the placement of a peripheral nerve catheter if a longer block duration is desired.
- The choice of local anesthetic is left to the practitioner performing the procedure, but various concentrations of bupivacaine or ropivacaine are typical. Other medications are sometimes added to the block solution to enhance the quality or extend the nerve block duration.
- Chlorhexidine 2% or povidone-iodine skin disinfectant solution
- An appropriate syringe with extension tubing
- Sterile ultrasound probe cover and gel
- ASA Standard monitors (non-invasive blood pressure monitoring, EKG, pulse oximetry)
Personnel
A single, qualified clinician can perform suprascapular nerve blocks. However, additional help may be required to properly position patients, provide sedation, or assist with the injection of local anesthetics.
Preparation
The process begins with obtaining informed consent from the patient. After the relevant risks, benefits, and alternatives have been explained, standard vital sign monitors are placed, and the patient can be positioned appropriately. An upright sitting position is ideal for the posterior approach to access the scapula and suprascapular notch. A reclined position is preferred for the anterior approach lateral to the supraclavicular brachial plexus. A blanket behind the patient’s shoulders can improve the visualization of the anatomy around the clavicle.
The skin overlying the block site should be widely prepped with 2% chlorhexidine and allowed to dry. A sterile ultrasound probe cover and gel should be used. The block solution can be drawn up into an appropriately sized syringe, connected to the block needle with extension tubing, and flushed to remove air from the system.
Technique or Treatment
The suprascapular nerve block can be performed on the posterior aspect of the shoulder at the suprascapular notch or via an anterior approach just lateral to the supraclavicular brachial plexus. Ultrasound guidance can be used to facilitate both techniques.
Anterior Suprascapular Nerve Block
Place the ultrasound transducer above the patient’s clavicle to begin to visualize the supraclavicular brachial plexus.
Trace the brachial plexus in the cephalad direction to the level of the cricoid cartilage (C6) to identify the interscalene brachial plexus between the anterior and middle scalene muscle.
The composition of the interscalene brachial plexus at this level is variable. Still, the three hypoechoic structures between the scalene muscles are usually the C5 nerve root on top and the C6 nerve root splitting in two. The C7 nerve root can also be present. Scan in the caudad directly, observing for a branch of C5 that moves laterally under the belly of the omohyoid muscle. This is the suprascapular nerve.
Follow the suprascapular nerve down towards the level of the supraclavicular brachial plexus, where it will be 1 to 3 centimeters lateral to the rest of the brachial plexus.
Utilize color doppler to identify any nearby vascular structures.
Insert the block needle with an in-plane approach from lateral to medial towards the suprascapular nerve. When below the omohyoid muscle and close to the nerve, confirm that the needle placement is extravascular by negative aspiration.
Inject a small amount (1 to 2 mL) of the block solution to verify appropriate needle tip placement and spread the solution around the suprascapular nerve. Continue to inject the block solution until adequate spread around the nerve is achieved, keeping in mind that the larger the volume injected, the higher the chance of phrenic nerve blockade.
Posterior Suprascapular Nerve Block
Place the ultrasound transducer above the spine of the patient’s scapula to visualize the trapezius and supraspinatus muscles.
Below these muscles, the scapula is seen as a hyperechoic line obscuring any deeper visualization. Ultrasound scanning of the surface of the scapula will reveal a slight depression of the bone known as the suprascapular canal.
Identify the suprascapular artery within this canal, using color doppler if possible. The suprascapular nerve runs alongside the artery.
An ideal location to block the suprascapular nerve is at the midpoint between the suprascapular notch and the spinoglenoid notch.
Insert the block needle with an in-plane approach from medial to lateral to avoid the acromion process laterally. Advance the needle through the trapezius and supraspinatus muscles until the tip of the needle is below the supraspinatus fascia and adjacent to the suprascapular artery and nerve.
Confirm that the needle is not intravascular by negative aspiration.
Inject a small amount (1 to 2 mL) of the block solution to verify appropriate needle tip placement and spread the solution around the suprascapular artery and nerve. Continue to inject the block solution until adequate spread around the nerve is achieved. If the nerve is not visualized (up to 27% of patients), inject 10 to 15 mL of block solution below the supraspinatus fascia.
Complications
Careful use of ultrasound with continuous visualization of the needle tip will reduce the risk of complications. Pneumothorax is a potential complication, occurring in about 1% of procedures, generally occurring by advancing the needle farther than needed.[14]
Thus, special care should be used in patients whose anatomy limits the visualization of the needle-point. Pneumothorax is a common cause of lawsuits in chronic pain practice, accounting for 4% of closed claim cases.[15] The risk of pneumothorax may be minimized by avoiding entering the suprascapular notch in the vertical plane. Positioning the ipsilateral hand to the contralateral shoulder will raise the scapula from the posterior chest wall and thus extend the separation between the skin and the chest wall, giving a more considerable margin of safety and reducing the risk of pneumothorax.[16]
Another risk of the suprascapular nerve block is an accidental intravenous or intraarterial injection. The suprascapular artery and vein lie near the nerve, even though they are separated by the superior transverse ligament of the scapula. The accidental puncture and injection into the vein or the artery could cause local anesthetic toxicity that may be fatal. Careful, frequent aspiration is necessary to avoid this complication. Visualization of local anesthetic spread on ultrasound also confirms non-vascular injection. The risk of intravascular injection increases in patients with poor ultrasound visualization.[17]
Other potential complications of peripheral nerve blocks, in general, include infection, bleeding, local anesthetic toxicity, and nerve injury.
Clinical Significance
Ultrasound-guided blockade of the suprascapular nerve is an effective method for treating acute and chronic shoulder pain. This nerve provides sensory innervation to both the acromioclavicular and glenohumeral joints. Two approaches to blocking the suprascapular nerve have been described, and their difference is clinically significant due to the proximity of the phrenic nerve to the brachial plexus. The posterior approach at the suprascapular canal has no risk of a phrenic blockade. The anterior approach is lateral to the brachial plexus, but the phrenic nerve can be affected depending on the volume of the block solution.
In a cadaver study investigating the phrenic sparing volume for the anterior suprascapular nerve block, a maximum volume of 4.2 mL was identified to dye the suprascapular nerve but spared the phrenic nerve 90% of the time (MEV90).[18] While further live human studies are needed to confirm the clinical significance of this cadaveric study, avoiding phrenic blockade is essential in patients with severe pulmonary disease.
The anterior blockade of the suprascapular nerve block may provide equivalent analgesia compared to the “gold standard” of the interscalene peripheral nerve block. A recent randomized prospective, a double-blinded study by Auyong et al. compared the analgesic benefit, opioid usage, and pulmonary compromise of three commonly used nerve blocks for shoulder surgery; the interscalene, supraclavicular, and suprascapular nerve block.[12]
The results suggested clinically comparable analgesia with dramatically different effects on lung function. The suprascapular and interscalene peripheral were essentially equivalent for analgesia (displaying clinically significant non-inferiority) and slightly outperformed the supraclavicular nerve block in pain scores. No clinically meaningful differences in opioid usage existed between the three groups. Interestingly, the patient’s pulmonary function was well preserved following the suprascapular nerve block, resulting in a vital capacity of 90% of the patient’s baseline, forced expiratory volume in 1 second (FEV1) of 87% of baseline, and reduced diaphragmatic excursion of 1.7 cm.
At the same time, the interscalene nerve block demonstrated a reduction of vital capacity to 67% of baseline, FEV1 of 68% of baseline, and diaphragmatic excursion reduction of 5.9 cm. This study strongly suggests that an anterior suprascapular nerve block provides analgesic equivalence to the interscalene block, with much improved pulmonary mechanics.[12]
Another recent prospective randomized double-blinded non-inferiority trial compared anterior suprascapular nerve block to interscalene block [19]. These authors also observed that the suprascapular nerve block is non-inferior to the traditional interscalene blockade. With similar analgesic results and improved pulmonary outcomes, both anterior and posterior approaches to the suprascapular nerve are valuable techniques in clinical practice.
Enhancing Healthcare Team Outcomes
As described in this article, an ultrasound-guided suprascapular nerve block can help treat many causes of acute and chronic shoulder pain. Before this procedure, a safety check or time-out can help ensure that the correct procedure is performed on the correct patient and that all necessary equipment is available. This is also an opportunity for the patient to ask any questions about the procedure that they might have after the informed consent process.
An appropriately trained anesthesia provider should perform the procedure, and a nurse or another anesthesia provider should be available to help. Another provider or nurse may also help monitor the patient's vital signs and administer sedation if necessary. Knowing the appropriate techniques and emphasizing clear communication between appropriate personnel will ensure patient safety around the time of the suprascapular nerve block.